Wound Assessment: Measuring Size, Type, Location, Age, And Severity For Optimal Treatment
Wounds are measured in several ways: size (area, depth, and dimensions), type (abrasion, laceration, etc.), location (anatomical region), age (acute, chronic), and severity (minor, moderate, major). Accurately measuring wound size is crucial for treatment planning, as it determines the appropriate dressings, medications, and frequency of wound care. Wound depth is also critical, as it classifies wounds as partial- or full-thickness, affecting treatment options and prognosis. Understanding wound type aids in identifying the underlying causes and predicting healing patterns. Wound location influences treatment strategies and healing outcomes due to variations in blood supply and skin characteristics. Wound age and severity guide treatment decisions, as they reflect the stage of healing and potential complications. Comprehensive wound assessment involves examination, documentation, and classification, providing a basis for individualized treatment plans and monitoring progress.
How Wounds Are Measured: A Comprehensive Guide
Wounds, those unwanted visitors that disrupt our skin’s integrity, come in various shapes, sizes, and depths. To embark on the healing journey effectively, it’s crucial to accurately measure these unwelcome guests. Here’s a detailed guide to demystify wound measurement techniques:
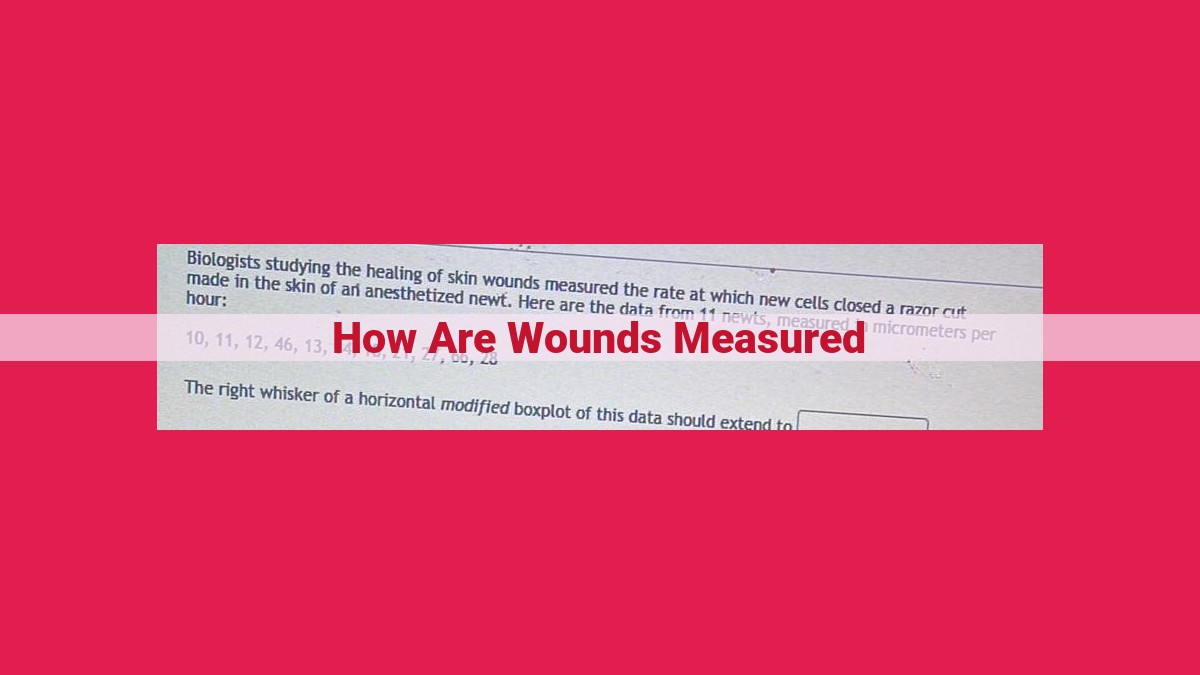
Measuring Wound Size
The surface area, length, and width of wounds provide valuable insights into their severity. Surface area, measured in square centimeters (cm²), helps determine the extent of damage and guides treatment decisions. Length and width, expressed in centimeters or millimeters (mm), provide a comprehensive understanding of the wound’s dimensions.
Determining Wound Depth
Wound depth classifies wounds into partial-thickness, full-thickness, or tunneling. Partial-thickness wounds involve damage to the epidermis and part of the dermis, while full-thickness wounds extend through all layers of the skin. Tunneling wounds are characterized by narrow channels or tracts beneath the skin’s surface. Wound depth significantly impacts treatment options and prognostication.
Exploring Wound Types
Understanding the various wound types is paramount for effective management. Abrasions are superficial injuries that involve the loss of the epidermis, while lacerations are cuts caused by sharp objects. Puncture wounds result from sharp objects piercing the skin, and incisions are intentional cuts made during surgery. Contusions, also known as bruises, are caused by blunt force trauma and are characterized by underlying bruising.
Identifying Wound Location
The location of a wound plays a crucial role in its assessment and treatment. Wounds near vital structures, such as blood vessels or nerves, require meticulous care. Anatomical landmarks and body parts provide essential context for understanding the wound’s proximity to sensitive areas.
Assessing Wound Age
Wounds progress through distinct stages of healing, classified based on their age: acute, chronic, and subacute. Acute wounds are recent injuries that typically heal within a few weeks. Chronic wounds persist for extended periods, often over several months, due to impaired healing. Subacute wounds fall between acute and chronic, transitioning from the inflammatory to the proliferative phase.
Classifying Wound Severity
Wounds are categorized as minor, moderate, or major based on their size, depth, and location. Minor wounds are superficial, usually less than 5 cm in length, and require minimal intervention. Moderate wounds are larger and deeper, involving partial-thickness damage or requiring closure with sutures or staples. Major wounds are extensive, full-thickness injuries that may require advanced medical treatment, including surgical intervention.
Explain the importance of accurately measuring wound size for treatment planning.
How Accurately Measuring Wound Size Impacts Treatment Planning
When it comes to wound care, understanding the size of the wound is crucial for devising an effective treatment plan. Accurately measuring wound size allows clinicians to:
- Determine the severity of the wound: Large wounds require more extensive treatment than smaller ones, as they have a greater potential for infection and complications.
- Estimate the amount of tissue damage: The size of the wound can help determine the extent of tissue damage, which influences the choice of dressings and therapies.
- Monitor wound healing progress: By tracking wound size over time, clinicians can assess the effectiveness of treatment and adjust it as needed.
Accurately measuring wound size involves using specific tools and techniques:
- Length and width: Measured using a ruler or measuring tape, these dimensions provide information about the overall surface area of the wound.
- Depth: Measured using a probe or caliper, the depth of the wound indicates the extent of tissue damage and can help determine if the wound is partial- or full-thickness.
- Surface area: Calculated by multiplying the length and width, the surface area provides a comprehensive measure of the wound’s size.
By precisely measuring wound size, clinicians gain valuable insights that guide treatment planning. They can determine the appropriate size of dressings, estimate the need for antibiotics or other medications, and monitor wound healing progression accurately. This informed approach ensures optimal wound healing outcomes, minimizes complications, and promotes patient well-being.
How Wounds Are Measured: A Comprehensive Guide
Wound Depth: Delving into the Layers of Injury
The depth of a wound is crucial in determining its severity and the appropriate treatment approach. Wounds are classified into three primary depth categories:
Partial-Thickness Wounds:
These wounds penetrate only the top layer of skin, known as the epidermis. They are often characterized by redness, pain, swelling, and superficial bleeding. Partial-thickness wounds typically heal quickly with minimal scarring.
Full-Thickness Wounds:
Full-thickness wounds extend through the epidermis and into the deeper layer of skin, called the dermis. They often appear as open wounds with visible tissue damage. These wounds require more extensive treatment and may result in scarring.
Tunneling Wounds:
Tunneling wounds are unique in that they extend beyond the visible surface area of the injury. They form narrow channels or tunnels that can reach deeper tissues or even bone. Tunneling wounds can be challenging to treat as they are difficult to clean and could lead to infection.
Understanding wound depth is essential for accurate assessment and effective wound management. By assessing the depth of a wound, healthcare professionals can determine the appropriate treatment plan, minimize the risk of complications, and promote optimal healing outcomes.
The Importance of Wound Depth in Treatment Planning
The depth of a wound significantly influences the treatment options and prognosis. Understanding wound depth allows healthcare professionals to customize a tailored treatment plan that promotes optimal healing and minimizes complications.
Partial-Thickness Wounds
These wounds penetrate only the superficial layers of the skin, leaving the underlying tissue intact. They are typically minor and heal relatively quickly with basic wound care. Treatment may involve cleaning the wound, applying bandages, and preventing infection.
Full-Thickness Wounds
In contrast, full-thickness wounds extend through all layers of the skin, exposing the underlying fat, muscle, or even bone. These wounds are more severe and require prompt medical attention. Treatment typically involves surgical closure, antibiotics, and specialized dressings to promote healing and prevent infection.
Tunneling Wounds
Tunneling wounds are a unique type of full-thickness wound that extends below the skin’s surface, creating a pocket of infection or debris. These wounds can be difficult to assess and treat, often requiring surgical exploration and extensive drainage.
How Wounds Are Measured: A Comprehensive Guide
Wounds can vary greatly in size, depth, type, and location. Accurately measuring these characteristics is crucial for proper treatment planning and optimal healing.
Wound Type: Abrasion, Laceration, Puncture, Incision, and Contusion
Abrasions are superficial injuries that involve only the top layer of skin (epidermis). They typically result from friction or scraping and appear as red, raw, or scraped areas.
Lacerations are deeper cuts that extend into the dermis (the second layer of skin). They are characterized by sharp, irregular edges and bleeding.
Puncture wounds are narrow, deep injuries caused by sharp objects like needles or nails. They can be particularly dangerous due to the potential for infection and damage to deeper tissues.
Incisions are clean, straight cuts made with a sharp instrument like a scalpel. They are often surgical wounds but can also be caused by accidents.
Contusions are bruises that result from blunt force trauma. They involve damage to blood vessels below the skin’s surface, causing discoloration and swelling.
Each wound type has unique characteristics that influence its healing process. Understanding these differences is essential for choosing the most effective treatment approach.
How Wounds Are Measured: A Comprehensive Guide
3. Wound Type: Abrasion, Laceration, Puncture, Incision, and Contusion
The type of wound you sustain depends on several factors, including the force, object, and body part involved. Understanding these factors helps determine the appropriate treatment and healing expectations.
Abrasions: These superficial wounds occur when the skin rubs against a rough surface, such as asphalt or carpet. Abrasions are usually minor but can be painful and prone to infection if not cleaned properly.
Lacerations: These wounds are caused by a sharp object, such as a knife or broken glass. Lacerations can be shallow or deep, and may require stitches or other treatments to close the wound.
Puncture Wounds: These are caused by a sharp, pointed object, such as a nail or needle. Puncture wounds can be deep and may damage underlying tissues or organs. It’s crucial to seek medical attention for proper cleaning and treatment to prevent infection.
Incisions: Unlike lacerations, incisions are straight, clean cuts made during surgery or other medical procedures. They typically require stitches or other methods to close the wound.
Contusions: Also known as bruises, contusions occur when blunt force impacts the body, causing blood vessels to break under the skin. The severity of contusions varies from minor to severe, depending on the force of the impact.
Each wound type has unique characteristics that influence healing. Abrasions and lacerations typically heal well with proper care. However, puncture wounds and contusions may require more attention to prevent complications such as infection or delayed healing. Understanding the factors that contribute to different wound types is essential for optimal healing and minimizing risks.
Wound Location: A Crucial Factor in Healing
Identifying the location of a wound is essential for accurate assessment and effective treatment. It helps healthcare providers determine the appropriate dressing, anticipate potential complications, and tailor the treatment plan to the specific anatomical region.
For instance, a wound on the face requires meticulous care to minimize scarring and preserve facial symmetry. In contrast, a wound on the leg may necessitate compression therapy to prevent edema and promote venous return.
Moreover, the location of a wound can affect the availability of blood supply and oxygen. Wounds located in areas with poor circulation, such as the extremities, may heal slower and be more prone to infection. Understanding the wound location allows providers to monitor the wound closely and adjust treatment accordingly.
Additionally, the location of a wound can provide clues about the underlying cause. Pressure ulcers, for example, are often found on bony prominences, while diabetic foot ulcers typically occur on the plantar surface of the foot. Understanding the location of a wound can help providers identify potential risk factors and implement preventive measures.
By identifying the wound location early on, healthcare professionals can develop a comprehensive treatment plan that addresses both the specific characteristics of the wound and the challenges posed by its anatomical position. This thorough approach enhances the chances of successful healing and reduces the risk of complications.
How Wound Location Impacts Treatment and Healing Outcomes
The location of a wound can significantly influence the treatment strategies employed and the healing prognosis. Wounds in certain areas of the body present unique challenges and may require specialized care.
For example, wounds on the face require meticulous attention due to their cosmetic implications. Surgical techniques aim to minimize scarring and preserve facial aesthetics. Wounds near the joints can impair mobility and may require physical therapy to restore range of motion. Wounds on the *feet must withstand the stress of weight-bearing, affecting the choice of dressings and healing time.
The ****anatomy**** of the wound site also plays a crucial role. Wounds on areas with abundant blood supply, such as the scalp, heal faster compared to wounds in areas with limited circulation, like the buttocks. Deeper wounds may damage underlying structures, necessitating more complex treatment and rehabilitation.
Moreover, wound location can affect the risk of infection. Wounds in areas prone to moisture or friction, like the armpits or groin, are more susceptible to bacterial growth. Wounds near organs or joints pose a higher risk of infection spreading to vital structures.
By understanding the unique characteristics of wounds in different locations, healthcare professionals can tailor treatment plans to optimize healing outcomes. Considering the wound’s location ensures appropriate wound care, minimizing complications, and expediting recovery.
How Wounds Are Measured: A Comprehensive Guide
Determining the extent of a wound is crucial for effective treatment and healing. Various factors are considered when measuring wounds, including size, depth, type, location, age, and severity. Understanding these aspects enables healthcare professionals to make informed decisions about wound care and minimize potential complications.
Wound Age: The Journey of Healing
Wounds progress through distinct stages of healing, each characterized by specific changes in the cellular and molecular processes. Based on the wound’s duration, they are classified as:
-
Acute Wounds: Occur suddenly and typically heal within a few weeks. They are characterized by inflammation, tissue repair, and the formation of new blood vessels.
-
Chronic Wounds: Persist for more than 12 weeks and exhibit impaired healing, often due to underlying medical conditions, infection, or poor circulation.
-
Subacute Wounds: Fall between acute and chronic wounds, lasting from 4 to 12 weeks. They may require more intensive care than acute wounds due to their delayed healing process.
Discuss the distinct characteristics and treatment approaches for acute, chronic, and subacute wounds.
Wound Age: The Journey from Acute to Chronic
Wounds, like our bodies, go through different stages in their healing journey. These stages are classified based on wound age: acute, chronic, and subacute.
Acute Wounds: The Fresh Start
Acute wounds are the newborns of the wound family, fresh and eager to heal. They appear within six weeks of injury and are characterized by inflammation, redness, and pain. The body’s defense system kicks into action, striving to restore the damaged tissue.
Chronic Wounds: The Prolonged Stall
Unlike their acute counterparts, chronic wounds linger beyond six weeks, stuck in a cycle of delayed healing. These persistent wounds often have underlying medical conditions or factors that hinder their progress, such as diabetes or poor circulation. They typically exhibit chronic inflammation, infection, and slow tissue repair.
Subacute Wounds: The In-Between Phase
Subacute wounds reside in the gray area between acute and chronic, lasting two to six weeks. They are not as fresh as acute wounds but not as stubborn as chronic ones. Subacute wounds may occur when an acute wound fails to heal within the typical timeframe and starts to develop signs of chronicity.
Distinct Characteristics and Treatment Approaches
Each wound age presents unique challenges and requires tailored treatment strategies.
- Acute Wounds:
- Goal: Promote rapid healing and minimize scarring.
- Treatment: Keep the wound clean, manage inflammation, and protect it from infection.
- Chronic Wounds:
- Goal: Manage underlying conditions, prevent infection, and stimulate tissue growth.
- Treatment: May involve wound debridement, antibiotics, hyperbaric oxygen therapy, or advanced wound dressings to promote healing.
- Subacute Wounds:
- Goal: Transition to acute healing or prevent progression to chronicity.
- Treatment: Includes a combination of acute and chronic wound care strategies, focusing on addressing underlying issues and facilitating tissue regeneration.
Understanding wound age is crucial for proper assessment, treatment planning, and monitoring. By recognizing the distinct characteristics and treatment approaches for acute, chronic, and subacute wounds, healthcare professionals can optimize wound healing outcomes and improve patient well-being.
How Wounds Are Measured: A Comprehensive Guide
Understanding the intricacies of wound measurement is crucial for effective assessment and treatment planning. Wound severity, a key aspect of classification, plays a vital role in determining the appropriate course of action.
Minor Wounds
These wounds are superficial, typically involving only the epidermis (outermost skin layer). They are usually caused by minor trauma, such as cuts or abrasions. Minor wounds are often characterized by minimal bleeding, pain, and swelling, and heal relatively quickly without complications.
Moderate Wounds
Moderate wounds penetrate deeper into the skin, affecting the dermis (middle skin layer). The edges of these wounds may be jagged or irregular, and they often bleed moderately. They can cause significant pain and swelling, and may take longer to heal than minor wounds. While they usually do not require extensive medical intervention, they should be properly cleaned and dressed to prevent infection.
Major Wounds
Major wounds extend beyond the dermis, involving the subcutaneous tissue (fat layer beneath the skin), muscles, or bones. These wounds are usually caused by severe trauma, such as accidents or surgical procedures. They often result in heavy bleeding, severe pain, and tissue damage. Immediate medical attention is essential to prevent complications and ensure proper healing.
Significance of Wound Severity Classification
Classifying wounds into minor, moderate, or major is not merely a labeling exercise. It has significant implications for treatment decisions and outcomes.
- Minor wounds may only require simple cleansing and bandaging.
- Moderate wounds may need stitches or other closure techniques, as well as antibiotics to prevent infection.
- Major wounds often require extensive surgical intervention, such as wound debridement (removal of damaged tissue) and suturing or skin grafting.
Accurate assessment of wound severity is therefore crucial for ensuring optimal healing and reducing the risk of complications. By understanding the criteria used to classify wounds, healthcare professionals can provide timely and appropriate care.
How Wounds Are Measured: A Comprehensive Guide
When you suffer a wound, it’s crucial to understand its severity for proper treatment and healing. Wound severity plays a significant role in determining the best course of action, as well as the potential outcomes.
Minor wounds are typically superficial and affect only the outermost layer of skin. They usually heal without complications and may only require basic wound care, such as cleaning and dressing.
Moderate wounds extend beyond the superficial layer but do not penetrate the entire thickness of the skin. These wounds may require more intensive treatment, such as antibiotics or stitches, to promote healing and prevent infection.
Major wounds involve deeper tissue damage and often require specialized medical attention. They can be life-threatening if not treated promptly and appropriately. Such wounds may require surgery, wound debridement, or extensive wound care to prevent serious complications.
The impact of wound severity on treatment decisions is evident. For instance, a minor wound may need only basic first aid, while a moderate wound may require antibiotics and sutures. In severe cases, surgical intervention may be necessary to repair damaged tissues, remove debris, and prevent infection.
Moreover, wound severity affects the likelihood of complications. Minor wounds generally heal without complications, whereas moderate wounds have a higher risk of infection, scarring, and delayed healing. Major wounds, due to their depth and extent, can lead to life-threatening complications such as sepsis, organ damage, or even death.
Knowing the severity of a wound helps healthcare professionals make informed decisions about the best course of treatment, the expected healing time, and the potential risks involved. This knowledge allows for personalized treatment plans that optimize outcomes and minimize the chances of complications.
How Wounds Are Measured: A Comprehensive Guide
Wound Size: Area, Dimensions, and Surface Area
Accurately measuring the surface area, length, width, and depth of wounds is crucial for effective treatment planning. Advanced techniques like laser scanning and photogrammetry provide precise data, but simpler tools like rulers and wound templates remain widely used.
Wound Depth: Partial-Thickness, Full-Thickness, and Tunneling
Wound depth determines treatment options and prognosis. Partial-thickness wounds involve only the top layer of skin (epidermis) and heal without scarring. Full-thickness wounds penetrate the entire skin layer, exposing deeper tissues and requiring specialized care. Tunneling wounds extend beneath the skin surface, making them difficult to clean and treat.
Wound Type: Abrasion, Laceration, Puncture, Incision, and Contusion
Different wound types result from various causes and have unique healing characteristics. Abrasions are superficial scrapes, while lacerations are cuts with irregular edges. Puncture wounds are narrow, deep wounds caused by sharp objects. Incisions are clean cuts made by surgical instruments. Contusions are bruises involving damage to underlying tissues without breaking the skin.
Wound Location: Anatomical Region and Body Part
Wound location plays a crucial role in treatment decisions. Wounds on the face or hands require meticulous care due to their visibility and functional importance. Wounds near joints may affect mobility, while those in moist areas pose higher infection risks.
Wound Age: Acute, Chronic, and Subacute
Wounds progress through different healing stages, classified by their age:
- Acute wounds are fresh and actively healing.
- Chronic wounds remain unhealed for an extended period (more than 4 weeks).
- Subacute wounds fall between acute and chronic stages, with signs of both active healing and delayed progress.
Wound Severity: Minor, Moderate, and Major
Wound severity influences treatment priorities and outcomes:
- Minor wounds are superficial and heal quickly.
- Moderate wounds may require medical attention to prevent infection or further damage.
- Major wounds are severe, involving substantial tissue loss or damage to critical structures.
Wound Assessment: Evaluation, Documentation, and Classification
Comprehensive wound assessment involves a thorough evaluation:
- Examination: Visual inspection, palpation, and wound probing determine the size, depth, and type of wound.
- Documentation: Accurate documentation of wound characteristics, including location, age, and severity, is essential for tracking progress and informing treatment decisions.
- Classification: Wounds are then classified based on their assessment findings to guide appropriate treatment and monitor healing.
How Wounds Are Measured: A Comprehensive Guide
7. Wound Assessment: Evaluation, Documentation, and Classification
Importance of Thorough Wound Assessment
A thorough wound assessment is paramount for optimal healing and prevention of complications.
Steps Involved
Examination: Involve meticulous observation and palpation of the wound to evaluate size, depth, type, and presence of infection.
Documentation: Accurate documentation of wound characteristics, including dimensions, depth, drainage, and surrounding tissue condition, is crucial for monitoring progress and adjusting treatment plans.
Classification: Proper classification of wounds (e.g., acute vs. chronic, minor vs. major) guides treatment decisions and determines necessary interventions.
Benefits of Accurate Assessment
-
Facilitates timely diagnosis of underlying conditions: Accurate assessment helps identify potential complications like infection or underlying medical conditions that require further investigation.
-
Optimizes treatment planning: Accurate measurement provides a solid foundation for selecting appropriate dressings, medications, and other interventions that promote healing.
-
Prevents complications: Early identification and treatment of complications, such as infection or tissue damage, minimizes the risk of long-term health consequences.
-
Improves patient outcomes: Comprehensive wound assessments empower healthcare providers to make informed decisions that enhance patient comfort, reduce pain, and accelerate healing time.
Thorough wound assessment is an essential step in wound care that lays the groundwork for effective treatment and optimal patient outcomes. Neglecting proper assessment can lead to delayed healing, increased risk of complications, and compromised patient well-being. Healthcare professionals must prioritize comprehensive wound assessments to ensure the best possible outcomes for their patients.