Trachea Anatomy: Pseudostratified Columnar Epithelium And Its Respiratory Functions
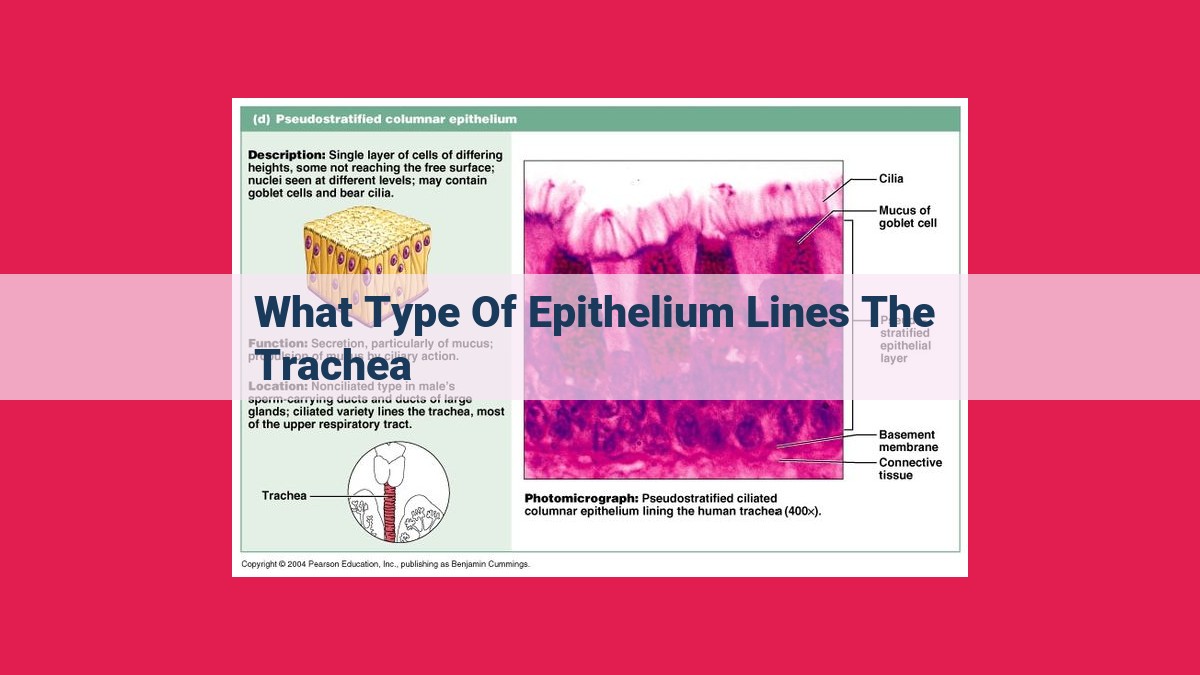
The trachea is lined by pseudostratified columnar epithelium, consisting of multiple cell layers with only some reaching the surface. Cilia on the epithelium’s surface propel mucus and debris away from the lungs, while goblet cells secrete mucus for protection. Clara cells aid in detoxification and repair. This epithelium is part of the respiratory mucosa, a protective lining of the respiratory tract.
Tracheal Epithelium: Pseudostratified Columnar Epithelium
- Description of the tracheal epithelium as pseudostratified columnar epithelium, with multiple cell layers but only some reaching the surface.
The Tracheal Epithelium: A Protective Barrier
The tracheal epithelium is a complex tissue that lines the trachea, the windpipe that carries air to and from the lungs. This pseudostratified columnar epithelium is like a protective blanket, with multiple layers of cells but only some reaching the surface.
Each layer plays a crucial role in keeping the trachea healthy and functioning properly.
Components of the Tracheal Epithelium
- Cilia: Tiny, hair-like projections that wave back and forth, propelling mucus and foreign particles out of the trachea.
- Goblet Cells: Specialized cells that produce and secrete mucus, creating a protective layer that traps and neutralizes irritants.
- Clara Cells: These non-ciliated cells are involved in detoxification, repair, and producing a surfactant that reduces surface tension in the lungs.
Related Concepts
Understanding the tracheal epithelium requires exploring some related concepts:
- Tracheal Glands: Located in the submucosa layer, these glands produce mucus that moistens the epithelium and helps remove debris.
- Respiratory Mucosa: The lining of the respiratory tract, consisting of pseudostratified columnar epithelium and underlying connective tissue.
- Mucous Membrane: A type of epithelial tissue found in body cavities exposed to the external environment. It contains goblet cells that produce mucus.
- Mucins: Glycoproteins that make up the main component of mucus.
- Acid Glycoproteins: Glycoproteins that contain sialic acid residues, contributing to the viscous properties of mucus.
- Bronchiolar Secretory Cells/Club Cells: Non-ciliated cells in bronchioles that produce surfactant to prevent lung collapse.
Together, these components work harmoniously to protect the tracheal epithelium from irritants, maintain moisture, and ensure the proper flow of air to and from the lungs.
The Tracheal Epithelium: A Guardian of Our Airways
Our trachea, or windpipe, plays a vital role in our respiratory system, allowing the passage of air to and from the lungs. Its lining, the tracheal epithelium, is a remarkable tissue that serves as a protective barrier, defense mechanism, and critical component in the respiratory process.
Layers of Protection: Pseudostratified Columnar Epithelium
The tracheal epithelium is categorized as pseudostratified columnar epithelium, a type of tissue characterized by multiple cell layers. However, despite having multiple layers, only certain cells are positioned to reach the surface, giving the appearance of a single cell layer. This strategic arrangement provides the trachea with added strength and resilience.
Guardians of the Airway: Components of the Tracheal Epithelium
The tracheal epithelium comprises an orchestra of specialized cells, each playing a vital role in maintaining the health and functionality of our airways:
Cilia: Imagine countless tiny, hair-like projections waving tirelessly within the trachea. These are cilia, the unsung heroes of our respiratory system. Their rhythmic beating motion propels mucus and trapped particles out of the trachea, clearing the airway of potential irritants and pathogens.
Goblet Cells: Intermingled with the cilia are goblet cells, the secretory powerhouses of the trachea. These specialized cells produce and release mucus, forming a protective blanket that lines the airway. This mucus layer traps foreign particles, including dust, bacteria, and viruses, preventing them from reaching the delicate lungs.
Clara Cells: Embedded within the tracheal epithelium are Clara cells, non-ciliated cells with a remarkable repertoire of functions. They contribute to detoxification, repairing damaged tissue, and producing surfactant, a substance that reduces surface tension within the airway, facilitating effortless breathing.
The tracheal epithelium is a marvel of cellular engineering, effectively guarding our airways against environmental hazards and facilitating unobstructed breathing. Cilia, goblet cells, and Clara cells work in perfect harmony to ensure the smooth functioning of our respiratory system, protecting us from infections and keeping our lungs healthy. Understanding the intricate workings of this protective layer enhances our appreciation for the complexity of our bodies and underscores the remarkable resilience of the human respiratory system.
Related Concepts
- Tracheal Glands: Mucus-producing glands located within the submucosa layer.
- Respiratory Mucosa: Lining of the respiratory tract, consisting of pseudostratified columnar epithelium and underlying connective tissue.
- Mucous Membrane: Epithelial tissue with goblet cells that produce mucus, lining body cavities exposed to the external environment.
- Mucins: Glycoproteins that form the main component of mucus.
- Acid Glycoproteins: Glycoproteins with sialic acid residues, contributing to the properties of mucins.
- Bronchiolar Secretory Cells/Club Cells: Non-ciliated cells found in bronchioles that produce surfactant to reduce surface tension.
The Trachea’s Defenses: A Closer Look at Its Epithelium and Related Structures
Nestled deep within your respiratory system lies a remarkable passageway called the trachea. This vital tube is lined with a specialized epithelium known as pseudostratified columnar epithelium that plays a crucial role in protecting your lungs.
Within this epithelium, a symphony of cells orchestrate a defense mechanism against inhaled particles and pathogens. Cilia, tiny hair-like structures, stand guard, waving their arms in unison to propel mucus and debris upwards towards the throat. Intermingled with the cilia are goblet cells, dedicated to producing and releasing mucus, a sticky substance that coats the trachea, trapping foreign particles and providing a moist environment.
Another unsung hero within the tracheal epithelium is the Clara cell. These non-ciliated cells are like cellular janitors, removing toxins and debris while also producing surfactants, a substance that helps keep the airway open.
Beyond the epithelium, the trachea relies on a network of tracheal glands to bolster its defenses. These glands, located beneath the epithelium, secrete additional mucus to enhance the protective barrier.
The tracheal epithelium is not an isolated entity but forms part of a larger system known as the respiratory mucosa. This lining extends throughout the respiratory tract, providing a continuous layer of protection against inhaled substances. Mucus membranes, which line body cavities exposed to the external environment, play a similar role, featuring goblet cells that produce mucus to guard against infections.
At the core of these protective mechanisms lies mucin, a glycoprotein that forms the very essence of mucus. Along with acid glycoproteins, which contribute to its unique properties, mucin forms a viscous barrier that traps and neutralizes potential threats.
In the deeper recesses of the respiratory tract, bronchiolar secretory cells take center stage. These non-ciliated cells, also known as club cells, reside in the bronchioles, producing surfactants that reduce surface tension, ensuring the airway remains open for efficient breathing.
Together, this intricate symphony of cells and structures safeguards your lungs, ensuring the smooth flow of air and protecting against harmful invaders. By understanding the complexities of the tracheal epithelium and its related components, we gain a deeper appreciation for the tireless efforts of our respiratory system to maintain our well-being.