Measure Tidal Volume And Other Lung Function Parameters Accurately With Spirometry
Tidal volume, a key lung function parameter, can be measured using spirometry, a non-invasive technique. During spirometry, patients forcibly exhale into a mouthpiece, and the volume of exhaled air over time is recorded. Tidal volume is the volume of air exhaled or inhaled during a normal breath and can be calculated from spirometry data. Related parameters like inspiratory capacity, expiratory reserve volume, vital capacity, peak expiratory flow rate, and forced expiratory volume in 1 second can also be measured using spirometry.
Understanding Lung Function: A Gateway to Respiratory Health
In the realm of respiratory health, understanding lung function is paramount. Our lungs, the tireless guardians of our breath, play a crucial role in gas exchange, absorbing life-giving oxygen and expelling harmful carbon dioxide. Spirometry, a non-invasive technique, offers us a valuable window into lung function, providing insights that can lead to better diagnosis and management of respiratory conditions.
Spirometry assesses various parameters, each reflecting a different aspect of lung function. These include tidal volume, the amount of air inhaled and exhaled with each breath; inspiratory capacity, the additional air we can inhale beyond tidal volume; and expiratory reserve volume, the air remaining in our lungs after normal exhalation.
Vital capacity, the maximum amount of air we can exhale after a deep inhalation, is another important parameter. Peak expiratory flow rate measures the maximum speed at which air can be expelled from the lungs, while forced expiratory volume in 1 second (FEV1) quantifies the amount of air exhaled in the first second of forced exhalation. These parameters provide a comprehensive assessment of lung function and can reveal abnormalities that may indicate respiratory problems.
Spirometry: A Comprehensive Overview
Understanding Lung Function
Your lungs are vital for your overall health, and understanding how well they function is crucial for maintaining respiratory well-being. Spirometry is a non-invasive technique that provides valuable insights into lung function, enabling healthcare professionals to diagnose and manage respiratory conditions effectively.
How Spirometry Works
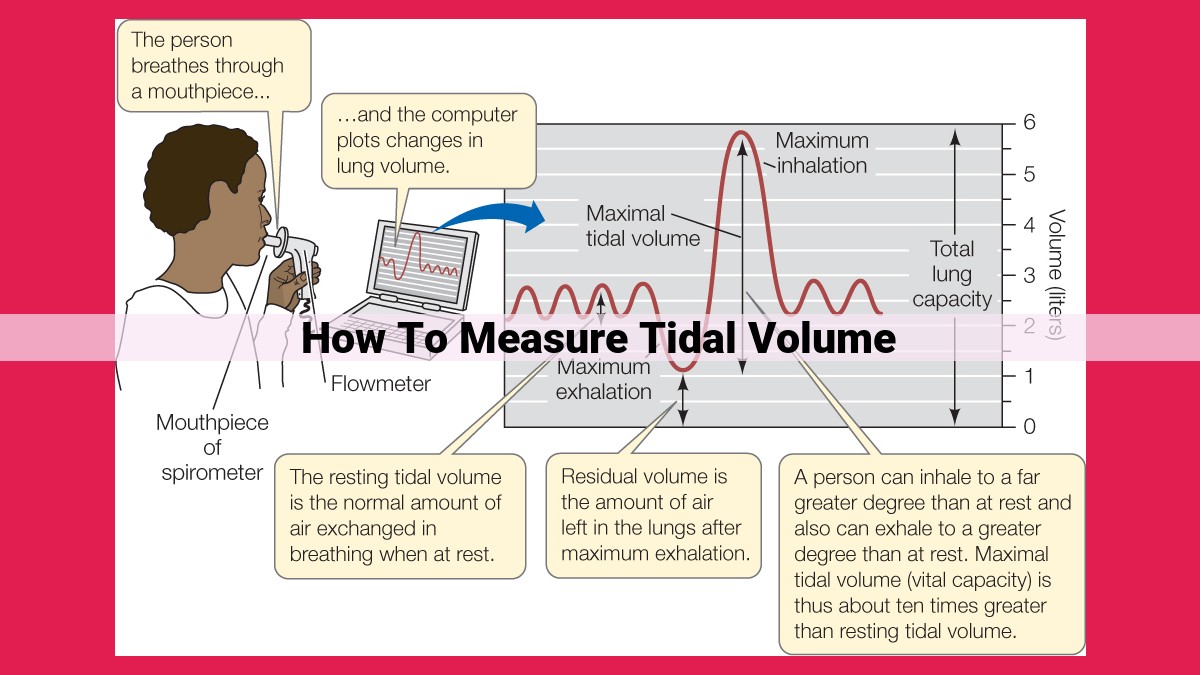
Spirometry involves measuring how much air you inhale and exhale and how fast you can move air out of your lungs. A spirometer, the device used for spirometry, records these measurements as you breathe into a mouthpiece connected to a computerized system.
Key Lung Function Parameters
Spirometry measures various lung function parameters, each providing specific information about your respiratory system.
- Tidal Volume: The amount of air you inhale or exhale during normal breathing.
- Inspiratory Capacity: The maximum amount of air you can inhale from the end of a normal exhalation.
- Expiratory Reserve Volume: The amount of air you can exhale after a normal exhalation.
- Residual Volume: The amount of air left in your lungs after a maximum exhalation.
- Vital Capacity: The maximum amount of air you can exhale after taking the deepest possible breath.
- Peak Expiratory Flow Rate: The fastest rate at which you can exhale air from your lungs.
- Forced Expiratory Volume in 1 Second (FEV1): The amount of air you can exhale in the first second of a forced exhalation.
Clinical Significance of Lung Function Parameters
Deviations from normal values of these parameters can indicate underlying respiratory conditions. For instance, reduced FEV1 and FEV1/FVC ratio may suggest obstructive lung diseases like asthma or COPD. Reduced vital capacity and impaired diffusion capacity may indicate restrictive lung diseases such as pulmonary fibrosis or interstitial lung disease. Decreased peak expiratory flow rate can be associated with impaired airway clearance in neuromuscular disorders.
Spirometry is a valuable tool in respiratory health, providing crucial information for diagnosing and managing lung conditions. By understanding the key lung function parameters measured by spirometry, you can gain a comprehensive picture of your respiratory health and take steps to maintain optimal lung function.
Measuring Tidal Volume and Related Parameters
Tidal Volume: The Breath of Life
Tidal volume is the volume of air that moves in and out of your lungs during normal breathing. Measuring tidal volume using spirometry involves breathing comfortably into a mouthpiece connected to a spirometer, a device that measures airflow and volume. The spirometer records the changes in air volume over time, giving us a graphical representation of your breathing pattern.
Inspiratory Capacity and Expiratory Reserve Volume: Expanding and Contracting
Inspiratory capacity is the additional volume of air you can inhale beyond tidal volume, usually during a deep breath. Expiratory reserve volume is the volume of air you can exhale beyond tidal volume, typically during a forced exhale. These parameters are calculated from the spirometry results, providing valuable insights into respiratory mechanics.
Vital Capacity: Your Breathing Symphony
Vital capacity is the total volume of air you can expel after taking the deepest possible breath. It encompasses both tidal volume and both reserve volumes. Measuring vital capacity helps us assess the overall capacity of your lungs to hold air, a crucial indicator of respiratory function.
Peak Expiratory Flow Rate: Expelling Air with Force
Peak expiratory flow rate is the maximum speed at which you can exhale. It’s measured during a forced exhale. This parameter reflects the strength of your respiratory muscles and the patency of your airways. Reduced peak expiratory flow rate may indicate conditions like asthma or chronic obstructive pulmonary disease (COPD).
Forced Expiratory Volume in 1 Second: A Window into Airways
Forced expiratory volume in 1 second (FEV1) is the volume of air you can exhale during the first second of a forced exhale. It’s an important diagnostic marker for obstructive lung diseases, such as COPD and asthma. Reduced FEV1 suggests airway narrowing, hindering airflow.
Clinical Significance of Lung Function Parameters
Understanding the clinical implications of lung function parameters is essential for accurate diagnosis and effective management of respiratory conditions. Spirometry, a non-invasive technique, provides valuable insights into these parameters, helping healthcare professionals assess lung function and identify potential underlying health issues.
-
Tidal volume: Variations from normal tidal volume can indicate respiratory abnormalities. Reduced tidal volume may suggest impaired ventilation, while increased tidal volume could indicate compensatory mechanisms to maintain adequate gas exchange.
-
Obstructive lung diseases: Reduced forced expiratory volume in 1 second (FEV1) and FEV1/forced vital capacity (FVC) ratio are hallmark features of obstructive lung diseases, such as asthma, chronic bronchitis, and emphysema. These parameters indicate airflow limitation due to airway narrowing or obstruction.
-
Restrictive lung diseases: Reduced vital capacity (VC) and impaired diffusion capacity are commonly associated with restrictive lung diseases, such as interstitial lung disease, pulmonary fibrosis, and sarcoidosis. These conditions restrict lung expansion and impede gas exchange.
-
Neuromuscular disorders: Decreased peak expiratory flow rate (PEFR) is often observed in individuals with neuromuscular disorders, such as muscular dystrophy and spinal cord injuries. Impaired airway clearance due to weakened respiratory muscles results in reduced airflow rates.
By understanding the clinical significance of lung function parameters, healthcare professionals can effectively interpret spirometry results and determine appropriate treatment strategies for respiratory conditions. Early detection and intervention can significantly improve patient outcomes and enhance overall respiratory health.