The Renal System: A Comprehensive Guide To Kidney Function, Blood Volume Regulation, And Blood Pressure Control
The kidneys regulate blood volume and blood pressure by controlling the filtration of blood through the glomeruli and the reabsorption and secretion of water and solutes in the renal tubules. Glomerular filtration rate (GFR) measures the amount of blood filtered, and filtration fraction determines how much fluid is reabsorbed. Active and passive mechanisms facilitate tubular reabsorption, while tubular secretion helps eliminate waste products. Renal plasma flow (RPF) provides the blood supply to the kidneys. Filtration surface area and glomerular capillary hydrostatic pressure drive filtration, while Bowman’s capsule hydrostatic pressure and blood colloid osmotic pressure oppose it. The nephron, especially the loop of Henle, DCT, and collecting duct, plays a crucial role in reabsorption and water concentration. Hormones like ADH and aldosterone regulate water and sodium reabsorption, respectively, and the renin-angiotensin-aldosterone system (RAAS) integrates hormonal responses to maintain blood volume and pressure.
The Kidneys: Masters of Blood Volume and Blood Pressure Regulation
Imagine your body as a finely tuned symphony, each organ playing a harmonious role in maintaining the delicate balance of life. Among these vital instruments, the kidneys stand as unsung heroes, silently and tirelessly ensuring the proper regulation of blood volume and blood pressure.
Their remarkable ability to filter impurities, conserve essential substances, and regulate fluid levels plays a pivotal role in our overall health and well-being. As we delve into the intricate workings of the kidneys, we will uncover the secrets behind their remarkable power to maintain the equilibrium of our delicate internal environment.
Glomerular Filtration Rate (GFR):
- Definition and importance of GFR as a measure of kidney function.
- Factors affecting GFR, such as glomerular capillary hydrostatic pressure, Bowman’s capsule hydrostatic pressure, and blood colloid osmotic pressure.
Glomerular Filtration Rate: The Kidney’s Measuring Stick for Health
Your kidneys are the unsung heroes of your body, working tirelessly to keep your blood clean and your fluids in balance. One of their most crucial functions is glomerular filtration rate (GFR), a measure of how well your kidneys are filtering waste and excess fluid from your blood.
Think of GFR as your kidney’s measuring stick. The higher your GFR, the better your kidneys are at filtering out toxins and maintaining your blood’s composition. But what exactly affects GFR, and why is it so important?
Factors that Influence GFR
Several factors can affect your GFR, including:
Glomerular Capillary Hydrostatic Pressure (PGC): The blood pressure inside the tiny blood vessels in your kidneys creates the force that pushes blood through the filtration barrier.
Bowman’s Capsule Hydrostatic Pressure (PBC): This is the pressure inside the capsule that surrounds the glomerular capillaries. It opposes the filtration force, preventing excessive fluid loss.
Blood Colloid Osmotic Pressure (π): The proteins in your blood create osmotic pressure, which draws fluid back into the blood vessels after filtration.
By carefully balancing these opposing forces, your kidneys ensure that essential substances stay in your bloodstream while waste products are filtered out.
Why GFR Matters
Maintaining a healthy GFR is vital for your overall health. When your GFR is too low, waste products can build up in your body, leading to kidney failure. Conversely, when your GFR is too high, your kidneys may not be able to filter out enough waste, resulting in electrolyte imbalances and other complications.
Monitoring your GFR is essential for early detection and management of kidney disease. Regular blood and urine tests can provide valuable insights into your kidney function, allowing your doctor to take appropriate measures to protect your kidneys and preserve your well-being.
Filtration Fraction: The Key to Understanding Fluid Balance
Imagine your kidneys as a sophisticated filtration system, responsible for maintaining the delicate balance of fluids in your body. Filtration fraction plays a crucial role in this process, determining how much fluid is filtered from your blood into the glomerular filtrate, the first step in urine formation.
The filtration fraction is essentially the percentage of blood plasma that is filtered by the kidneys per minute. It’s calculated by dividing the glomerular filtration rate (GFR) by the renal plasma flow (RPF). GFR is a measure of how much blood is filtered through the glomeruli, while RPF is the volume of blood flowing through the kidneys.
The filtration fraction typically ranges from 15-20%. This means that for every 100 milliliters of blood plasma entering the kidneys, 15-20 milliliters are filtered into the glomerular filtrate.
The significance of filtration fraction lies in its ability to influence how much fluid is reabsorbed or secreted by the tubules. If the filtration fraction is too high, excessive fluid may be lost from the body, leading to dehydration. Conversely, a low filtration fraction can result in fluid retention and swelling.
Overall, filtration fraction is a vital parameter that helps ensure optimal fluid balance in the body. By understanding this concept, we gain a deeper appreciation for the intricate workings of our kidneys and their essential role in maintaining overall health and well-being.
Tubular Reabsorption:
- Active and passive mechanisms involved in reabsorbing essential substances from the glomerular filtrate back into the bloodstream.
- Key role of the proximal tubule, loop of Henle, and distal convoluted tubule in reabsorption.
Tubular Reabsorption: The Kidneys’ Unsung Heroes
In the realm of our intricate biological machinery, the kidneys stand as masters of fluid regulation, ensuring a delicate balance within our bodies. They accomplish this through a series of intricate processes, one of which is tubular reabsorption.
Picture the glomerulus, a tiny filtering unit within each kidney, which separates essential substances from waste products. The resulting fluid, known as the glomerular filtrate, then travels through a series of tubules. Within these tubules, cells perform the crucial task of reabsorbing essential substances back into the bloodstream.
This vital process occurs through active and passive mechanisms. Active mechanisms use energy to transport substances against a concentration gradient, while passive mechanisms facilitate transport down a concentration gradient.
The proximal tubule, the first segment of the tubule system, is responsible for reabsorbing a vast majority of substances, including glucose, amino acids, and water. The loop of Henle plays a crucial role in concentrating urine, creating an osmotic gradient that drives water reabsorption. Finally, the distal convoluted tubule regulates fine-tuning of the remaining substances, particularly sodium and potassium.
These three segments work in concert, ensuring the body’s vital nutrients and fluids are preserved while waste products are eliminated.
Tubular Secretion:
- Process by which the kidneys actively transport certain substances from the bloodstream into the glomerular filtrate.
- Importance of tubular secretion in regulating pH balance and eliminating waste products.
Tubular Secretion: The Kidneys’ Secret Weapon for Maintaining Health
Imagine your kidneys as a sophisticated water filtration system, but with a secret weapon up their sleeve: tubular secretion. This process is like a special delivery service that actively transports certain substances from the bloodstream into the glomerular filtrate, the fluid produced during the initial stage of filtration.
Why is Tubular Secretion Important?
Tubular secretion plays a crucial role in maintaining the body’s delicate balance. It helps:
- Regulate pH balance: By transporting hydrogen ions (H+) into the filtrate, the kidneys can adjust the pH of the blood, ensuring it remains within a narrow range necessary for optimal functioning.
- Eliminate waste products: The kidneys use tubular secretion to excrete creatinine, a waste product of muscle metabolism, as well as other harmful substances that need to be removed from the body.
How Tubular Secretion Works
Tubular secretion is a highly selective process, controlled by specialized cells in the renal tubules. These cells use energy to actively transport certain substances against their concentration gradient, moving them from the bloodstream into the filtrate. This process ensures that these substances are removed from the body via the urine.
Key Substances Secreted by the Kidneys
The kidneys primarily secrete three types of substances:
- Hydrogen ions: Regulate pH balance
- Creatinine: Waste product of muscle metabolism
- Drugs and toxins: Excreted to protect the body
Interactions with Other Renal Processes
Tubular secretion is closely linked to other processes in the kidneys, such as glomerular filtration (the initial filtration of blood) and tubular reabsorption (the reabsorption of essential substances from the filtrate back into the bloodstream). These processes work together to fine-tune the composition of the urine and maintain the body’s overall fluid and electrolyte balance.
Tubular secretion is a crucial component of the kidneys’ filtration system. By actively transporting certain substances into the glomerular filtrate, the kidneys help regulate pH balance, eliminate waste products, and protect the body from harmful substances. Understanding this process highlights the remarkable complexity and importance of the kidneys in maintaining our health and well-being.
Renal Plasma Flow: The Kidney’s Blood Circulation
The Kidneys: Master Regulators of Blood Volume and Pressure
Our kidneys are remarkable organs that play a pivotal role in maintaining our overall health, primarily by regulating blood volume and blood pressure. One of the key components of this intricate regulatory system is renal plasma flow (RPF), the volume of blood flowing through the kidneys per minute.
Understanding RPF’s Relationship with GFR and Filtration Fraction
RPF is closely linked to glomerular filtration rate (GFR), which measures the amount of fluid filtered from the blood into the Bowman’s capsule. Filtration fraction, on the other hand, indicates the proportion of plasma that is filtered out during this process.
These three variables are interconnected:
- High RPF leads to increased GFR, which allows for the filtration of a greater volume of fluid.
- Low RPF results in decreased GFR, reducing the amount of fluid filtered.
- Filtration fraction is determined by the ratio of GFR to RPF, typically ranging between 0.15 and 0.25.
Exploring the Significance of RPF
Comprehending RPF is essential because it provides insights into:
- Kidney function: RPF reflects the kidneys’ ability to receive blood and filter waste products.
- GFR estimation: RPF can be used to indirectly estimate GFR, a crucial indicator of kidney health.
- Renal blood flow regulation: RPF is regulated by various mechanisms, including hormonal signals and autoregulation.
Maintaining RPF for Optimal Health
Optimal RPF is crucial for kidney health and overall well-being. Factors that can affect RPF include:
- Blood pressure: Low blood pressure can reduce RPF, while high blood pressure can damage the kidneys’ blood vessels.
- Kidney health: Kidney disease can significantly impair RPF and lead to complications.
- Medications: Certain medications can alter RPF, so consultation with a healthcare professional is essential.
Renal plasma flow is a fundamental aspect of the kidneys’ function. Understanding its relationship with GFR and filtration fraction is essential for assessing kidney health and maintaining overall well-being. By ensuring optimal RPF, we support our kidneys’ ability to effectively filter waste products, regulate blood volume, and maintain a healthy blood pressure.
Filtration Surface Area: The Key to Efficient Kidney Function
In the intricate world of human physiology, the kidneys stand as remarkable organs responsible for maintaining the delicate balance of blood volume and blood pressure. At the heart of this process lies the filtration surface area, an extensive network that ensures the efficient filtration of waste products and excess fluids from the bloodstream.
Think of it as a vast molecular sieve, where millions of tiny filters, known as nephrons, work tirelessly to separate essential substances from waste. Each nephron begins with a specialized structure called the glomerulus, a cluster of tiny blood vessels that form the initial filtration barrier. As blood flows through the glomerulus, fluid and small molecules are forced into the Bowman’s capsule, the first part of the nephron. Here, the filtration surface area plays a pivotal role.
The magnitude of this surface area is truly remarkable, providing ample space for the filtration process to occur. Each kidney contains approximately one million nephrons, each with its own filtration surface area. This extensive network allows for a maximum exchange of fluids and solutes, ensuring that vital substances remain in the bloodstream while waste products are directed towards elimination.
Factors such as the number of nephrons and the size of the glomerular capillaries influence the filtration surface area. In individuals with a reduced number of nephrons or smaller glomerular capillaries, the overall filtration efficiency may be compromised, leading to potential health concerns.
Understanding the role of the filtration surface area is crucial for appreciating the kidneys’ remarkable ability to maintain blood volume and blood pressure. Its intricate design ensures that essential fluids and molecules are retained, while waste products are effectively removed, contributing to our overall health and well-being.
Glomerular Capillary Hydrostatic Pressure (PGC): The Driving Force Behind Filtration
The kidneys play a crucial role in regulating blood volume and blood pressure, and one of the key determinants of their filtering capacity is glomerular capillary hydrostatic pressure (PGC). PGC is the force that drives the filtration of blood through the glomerulus, the tiny filtering unit within each kidney.
Blood pressure is the main factor that determines PGC. Blood pressure creates a gradient that forces fluid and solutes out of the glomerular capillaries and into Bowman’s capsule, the cup-shaped structure that surrounds the glomerulus.
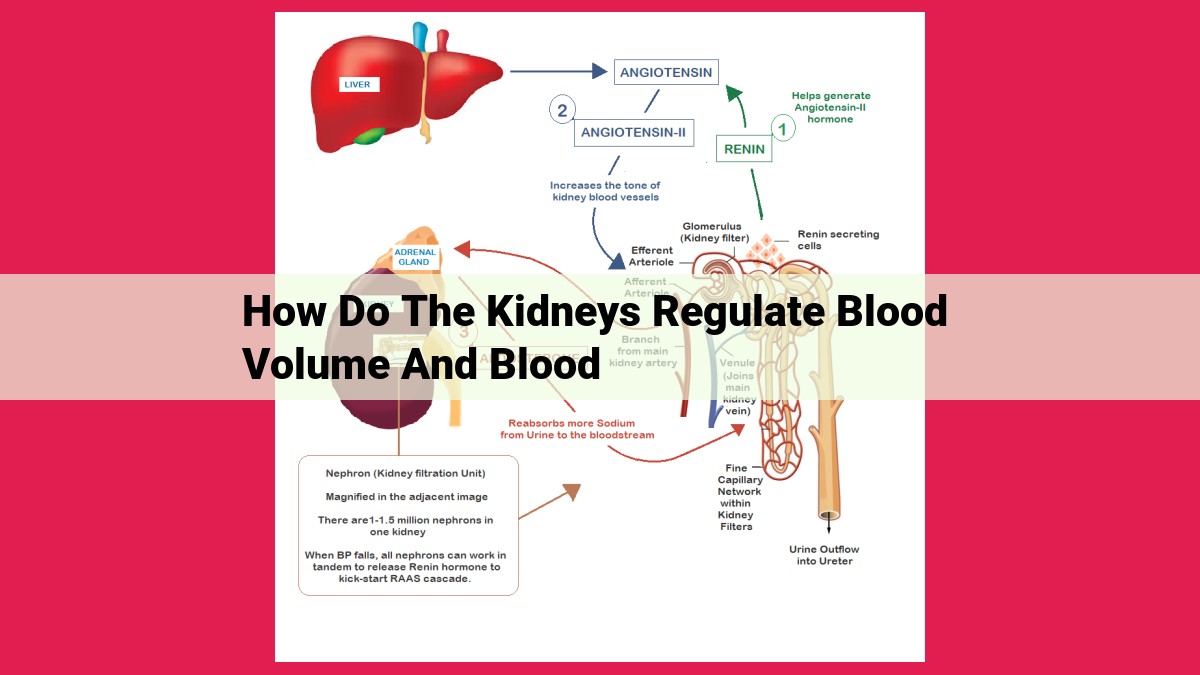
PGC is tightly regulated by the renin-angiotensin-aldosterone system (RAAS) to ensure optimal filtration. When blood pressure drops, RAAS triggers the release of renin, which in turn converts angiotensin I into angiotensin II. Angiotensin II then stimulates the release of aldosterone, which promotes sodium reabsorption in the distal convoluted tubule and collecting duct. This results in increased water reabsorption, which in turn increases blood volume and blood pressure.
Conversely, when blood pressure is too high, RAAS is inhibited, reducing PGC and decreasing filtration. This helps to lower blood pressure by reducing the volume of fluid circulating in the bloodstream.
Understanding the role of PGC in filtration is essential for maintaining overall kidney health and blood pressure regulation. By optimizing PGC, the kidneys can efficiently filter waste products from the blood while maintaining the proper balance of fluids and electrolytes in the body.
Bowman’s Capsule Hydrostatic Pressure: The Unsung Hero of Fluid Balance
Within the intricate machinery of our kidneys, a delicate dance unfolds between opposing forces, ensuring the precise orchestration of fluid filtration. One such force, Bowman’s capsule hydrostatic pressure (PBC), plays a crucial yet often overlooked role in safeguarding our body’s delicate fluid balance.
PBC is a counteracting force that opposes the powerful glomerular capillary hydrostatic pressure (PGC), the driving force behind fluid filtration in the glomerulus. Imagine a tiny tug-of-war within the kidney’s filtration unit, with PGC pulling fluid out of the blood and PBC pulling it back in.
The significance of PBC lies in its ability to prevent excessive fluid loss. Without this countervailing force, fluids would rush out of the glomerulus unchecked, potentially leading to dehydration and electrolyte imbalances. PBC therefore acts as a safety mechanism, ensuring that only the necessary amount of fluid is filtered for subsequent reabsorption and utilization by the body.
Maintaining an optimal PBC is essential for proper kidney function. Factors such as kidney disease, heart failure, and obstruction of the urinary tract can disrupt this delicate balance, leading to abnormal fluid filtration and potential health complications.
In the context of kidney function, Bowman’s capsule hydrostatic pressure is an indispensable player, quietly working behind the scenes to ensure the body’s fluid homeostasis. Understanding its role not only enhances our appreciation for the intricacies of the human body but also underscores the importance of kidney health for overall well-being.
Blood Colloid Osmotic Pressure (π): The Silent Regulator of Filtration
When you think of the kidneys, you probably imagine them filtering waste products from your blood. But did you know that they also play a crucial role in regulating your blood volume and blood pressure? And one of the key players in this process is something called colloid osmotic pressure (π).
Colloid osmotic pressure is the pressure exerted by large molecules, known as colloids, in a fluid. In our blood, these colloids are mainly proteins, such as albumin and globulins. These proteins are too large to pass through the tiny pores in the glomerular capillaries, the microscopic blood vessels where filtration occurs.
As blood flows through the glomerular capillaries, water and small molecules are pushed out into Bowman’s capsule, the cup-shaped structure surrounding the capillaries. This process, known as glomerular filtration, helps remove waste products and excess fluid from the blood. However, some of this fluid needs to be reabsorbed back into the bloodstream to maintain proper hydration.
This is where colloid osmotic pressure comes into play. As the filtered fluid moves through the proximal tubules (the first section of the kidney tubules), the reabsorption of essential substances like glucose and amino acids creates a concentration gradient. This gradient draws water back into the bloodstream through a process called osmosis.
Colloid osmotic pressure is particularly important in the peritubular capillaries, which run alongside the tubules. The high concentration of proteins in the blood creates an osmotic pressure that pulls fluid out of the tubules and back into the capillaries. This process ensures that enough fluid is returned to the bloodstream to maintain blood volume and blood pressure.
Without adequate colloid osmotic pressure, too much fluid would be lost through filtration, leading to dehydration and low blood pressure. Conversely, if colloid osmotic pressure is too high, it can hinder filtration and lead to fluid retention and high blood pressure.
Maintaining a healthy balance of colloid osmotic pressure is crucial for the kidneys to properly regulate blood volume and blood pressure. This delicate balance is maintained through the complex interplay of hormones, such as antidiuretic hormone (ADH) and aldosterone, and the kidneys’ ability to adjust filtration and reabsorption rates.
The next time you think of your kidneys, remember that they are not just waste-removing machines. They are also master regulators of your blood’s composition and volume, and colloid osmotic pressure is one of their unsung heroes.
Nephron: The Functional Unit of the Kidney:
- Structure and function of the nephron, including the glomerulus, Bowman’s capsule, proximal tubule, loop of Henle, distal convoluted tubule, and collecting duct.
The Nephron: The Kidneys’ Microscopic Marvel
Nestled within the kidneys’ intricate network lies the nephron, a microscopic powerhouse responsible for the kidneys’ extraordinary ability to regulate blood volume and blood pressure. Each kidney houses millions of these tiny units, working tirelessly to maintain the delicate balance of our internal environment.
Structure of the Nephron
The nephron is an awe-inspiring feat of biological engineering. It consists of several interconnected segments, each playing a crucial role in the intricate process of urine formation:
- Glomerulus: Acts as a filter, allowing fluid and waste products from the blood to pass into a cup-shaped structure called Bowman’s capsule.
- Bowman’s capsule: Surrounds the glomerulus, collecting the filtered fluid and sending it to the rest of the nephron.
- Proximal tubule: Reabsorbs essential nutrients, water, and ions from the filtered fluid back into the bloodstream.
- Loop of Henle: A U-shaped segment that creates an osmotic gradient, concentrating the urine by reabsorbing water and excreting ions.
- Distal convoluted tubule (DCT): Further regulates water and electrolyte reabsorption, influencing blood pH and potassium levels.
- Collecting duct: The final destination, where water and solutes are reabsorbed or excreted under the influence of antidiuretic hormone (ADH).
Function of the Nephron
The nephron’s primary function is to filter waste products from the blood and regulate fluid and electrolyte balance. Through a series of intricate processes, the nephron helps maintain optimal blood pressure, electrolyte levels, and pH balance:
- Filtration: In the glomerulus, blood pressure forces fluid and waste products out of the bloodstream into Bowman’s capsule.
- Reabsorption: Essential substances are actively and passively reabsorbed from the filtered fluid back into the bloodstream in the proximal tubule, loop of Henle, and DCT.
- Secretion: Some waste products are actively transported from the bloodstream into the filtered fluid in the proximal tubule and DCT.
- Excretion: The remaining waste products and excess water are eliminated from the body as urine.
The nephron, a remarkable masterpiece of biological engineering, stands as a testament to the intricate workings of the human body. Its tireless function in regulating blood volume and blood pressure ensures our overall health and well-being. By understanding the remarkable role of the nephron, we can appreciate the profound importance of maintaining kidney health for a long and healthy life.
Loop of Henle:
- Unique structure and role in concentrating the urine by creating an osmotic gradient.
The Loop of Henle: A Masterpiece in Urine Concentration
In the heart of our kidneys lies a remarkable structure called the Loop of Henle, a vital component in the intricate symphony of urine formation. This U-shaped structure, with its ascending and descending limbs, plays a crucial role in transforming a dilute filtrate into a concentrated urine.
The Loop of Henle’s unique design creates an osmotic gradient, a gradual increase in solute concentration, which drives the reabsorption of water. As the filtrate descends into the Loop’s descending limb, water is reabsorbed into the bloodstream, leaving behind a more concentrated filtrate.
Upon reaching the Loop’s hairpin turn, the concentrated filtrate enters the ascending limb. Here, the active transport of sodium ions out of the tubule creates an osmotic gradient that favors the reabsorption of water from the interstitial fluid surrounding the Loop. This process effectively strips the filtrate of water, leaving behind a hypertonic urine.
The Loop of Henle’s ability to concentrate urine is essential for several reasons. It allows the kidneys to excrete excess solutes without losing excessive water, which would lead to dehydration. It also plays a role in maintaining blood pressure by regulating the volume of extracellular fluid.
Furthermore, the Loop of Henle’s concentrating mechanism is crucial for desert-dwelling animals that must conserve water. Without this adaptation, these animals would be highly vulnerable to dehydration.
In conclusion, the Loop of Henle is a remarkable example of nature’s ingenuity. Its intricate structure and functional capabilities allow the kidneys to perform the essential task of urine concentration, ensuring our survival and maintaining a healthy balance of fluids and solutes in the body.
Distal Convoluted Tubule (DCT):
- Function in regulating acid-base balance and water reabsorption.
The Distal Convoluted Tubule: A Vital Player in Kidney Function
In the intricate workings of the kidneys, the distal convoluted tubule (DCT) plays a pivotal role in maintaining our pH balance and ensuring proper water reabsorption. As part of the nephron, the functional unit of the kidneys, the DCT is a specialized section where vital adjustments take place to optimize our body’s fluid and electrolyte levels.
Regulating Acid-Base Balance
The DCT is responsible for regulating the pH level of our blood. By selectively secreting hydrogen ions (H+) or bicarbonate ions (HCO3-), the DCT can either acidify or alkalize the urine. This function is crucial for maintaining a healthy pH range in the body, ensuring that our cells and tissues function optimally.
Optimizing Water Reabsorption
The DCT also plays a critical role in regulating water reabsorption. By controlling the permeability of the tubule wall, the DCT can increase or decrease the amount of water that is reabsorbed back into the bloodstream. This process is essential for maintaining fluid balance and preventing dehydration.
Hormonal Control of the DCT
The DCT’s functions are regulated by a variety of hormones, including antidiuretic hormone (ADH) and aldosterone. ADH increases the permeability of the DCT, allowing more water to be reabsorbed and thus reducing urine output. Aldosterone, on the other hand, promotes the reabsorption of sodium ions, which indirectly influences water reabsorption.
Implications for Health
Understanding the role of the DCT is essential for maintaining overall health and well-being. Impaired function of the DCT can lead to electrolyte imbalances, dehydration, and pH disturbances, all of which can have serious consequences for the body. Therefore, preserving the health of our kidneys and the DCT is crucial for our long-term health and vitality.
The Collecting Duct: A Master Regulator of Water Balance
In our intricate symphony of life, the kidneys emerge as masterful conductors, orchestrating the delicate dance of blood volume and blood pressure. Among their many vital functions, the kidneys are the gatekeepers of our fluid balance, ensuring that our bodies maintain the optimal levels of hydration. At the heart of this delicate operation lies the collecting duct, the final stage in the renal filtration process.
Collecting Duct: The Ultimate Control Center
The collecting duct is no ordinary structure. It is the final frontier where water and solutes are meticulously reabsorbed, ensuring that our bodies retain the fluids we need while flushing out waste products. This critical function is overseen by a powerful hormone called antidiuretic hormone (ADH).
ADH acts like a wise commander, skillfully regulating water reabsorption in the collecting duct. When blood osmolality rises, signaling a decrease in body water, ADH is released. This hormone instructs the collecting ducts to become more permeable to water, allowing for increased reabsorption. As a result, the body conserves precious water, preventing dehydration.
ADH: The Guardian of Blood Osmolality
Blood osmolality, a measure of the concentration of dissolved particles in the blood, is closely monitored by the body. ADH ensures that blood osmolality remains within a narrow range, safeguarding our cells from dehydration or excessive swelling. Without ADH, our bodies would struggle to maintain a healthy water balance.
The collecting duct, under the watchful eye of ADH, plays a pivotal role in regulating blood volume and blood pressure. Its ability to control water reabsorption is crucial for maintaining our body’s fluid balance, a cornerstone of overall health. Understanding these intricate mechanisms helps us appreciate the remarkable symphony of our bodies and the vital role the kidneys play in our well-being.
Antidiuretic Hormone (ADH): The Guardian of Blood Osmolality
Imagine your body as a finely tuned orchestra, where every instrument plays a crucial role in maintaining harmony. Your kidneys are the conductors of this orchestra, orchestrating the delicate balance of fluid and electrolytes that keep you functioning optimally. Among their many duties, the kidneys boast a remarkable ability to regulate blood volume and blood pressure through a sophisticated system involving a hormone known as antidiuretic hormone (ADH).
Nestled in the hypothalamus of your brain, ADH acts as a vigilant sentinel, monitoring the osmolality of your blood. Osmolality refers to the concentration of particles, like sodium and glucose, dissolved in your blood. When blood osmolality rises, indicating dehydration, ADH springs into action. It travels through the bloodstream to the collecting ducts of your kidneys, the final stop in the urine formation process.
In the collecting ducts, ADH stimulates the insertion of aquaporins into the cell membranes. These channels act like tiny doors, allowing water to diffuse out of the collecting ducts and back into the bloodstream. As water is reabsorbed, the urine becomes more concentrated, carrying away waste products while conserving precious fluid. This process contributes to maintaining a normal blood osmolality.
Conversely, when blood osmolality drops due to excessive water intake, ADH secretion is suppressed. Without ADH, aquaporins are not inserted into the collecting ducts, and water is freely excreted in the urine. This results in a more dilute urine and helps restore blood osmolality to normal levels.
ADH’s role in fluid balance is critical for maintaining blood pressure. When blood volume decreases due to dehydration or blood loss, ADH helps conserve water, increasing circulating blood volume and restoring blood pressure. Conversely, when blood volume is excessive, ADH secretion is suppressed, leading to increased urine output and a decrease in blood pressure.
In summary, ADH is an essential hormone that regulates water reabsorption in the kidneys, maintaining blood osmolality and blood pressure. Its ability to adapt to changing fluid status highlights the remarkable complexity of the kidney’s role in ensuring our overall health and well-being.
Aldosterone:
- Hormone that regulates sodium reabsorption in the distal convoluted tubule and collecting duct.
- Role of aldosterone in blood pressure regulation.
Aldosterone: The Silent Guardian of Blood Pressure
Within the intricate workings of our bodies, hormones play a pivotal role as messengers, orchestrating the precise regulation of numerous physiological processes. Among these unsung heroes, aldosterone stands as a silent guardian, tirelessly safeguarding our blood pressure and ensuring the delicate balance of electrolytes within our bodies.
Produced by the adrenal glands, aldosterone acts on the distal convoluted tubule and collecting duct of the kidneys, stimulating the reabsorption of sodium and water back into the bloodstream. This interplay of aldosterone and the kidneys holds immense significance for maintaining proper blood pressure and fluid balance.
When blood pressure drops, the kidneys release renin, an enzyme that triggers a cascade of events leading to the production of angiotensin II. This potent hormone stimulates the adrenal glands to release aldosterone, which in turn increases sodium and water reabsorption. The increased volume of fluid in the bloodstream elevates blood pressure back to normal levels.
Aldosterone’s role extends beyond blood pressure regulation. It also influences the body’s electrolyte balance by controlling potassium excretion. As aldosterone increases sodium reabsorption, it simultaneously promotes potassium secretion into the urine. This intricate interplay ensures that potassium levels remain within a narrow range necessary for proper cellular function.
Understanding aldosterone’s actions is crucial for comprehending various medical conditions. For instance, excessive aldosterone production (known as aldosteronism) can lead to high blood pressure, while insufficient aldosterone (called hypoaldosteronism) can cause hypotension and life-threatening electrolyte imbalances.
In conclusion, aldosterone is an essential hormone that silently ensures the proper regulation of blood pressure and fluid balance. Its delicate interplay with the kidneys and other hormonal systems highlights the complexity and resilience of our bodies. Recognizing the importance of aldosterone’s actions empowers us to appreciate the intricate mechanisms that maintain our well-being.
The Renin-Angiotensin-Aldosterone System (RAAS): A Vital Regulator of Blood Volume and Blood Pressure
In the intricate symphony of our bodies, the kidneys play a pivotal role in maintaining the delicate balance of blood volume and blood pressure. The renin-angiotensin-aldosterone system (RAAS), a complex hormonal network, collaborates closely with the kidneys to ensure this delicate equilibrium is harmoniously preserved.
The RAAS Cascade: A Chain Reaction
Picture a domino effect, each step triggering the next. This is precisely how RAAS operates. When blood volume or blood pressure dips, a specialized enzyme called renin is released by the kidneys. Renin initiates a cascade of reactions, converting a protein called angiotensinogen into its active form, angiotensin I.
Angiotensin I encounters an enzyme called angiotensin-converting enzyme (ACE), primarily found in the lungs. ACE further transforms it into angiotensin II, a potent vasoconstrictor. As its name suggests, angiotensin II constricts blood vessels, causing a rise in blood pressure.
Sodium Reabsorption: Aldosterone’s Contribution
But RAAS has another key player: aldosterone. This hormone, secreted by the adrenal glands, stimulates the kidneys to reabsorb more sodium. Increased sodium reabsorption leads to increased water retention, further boosting blood volume.
GFR Modulation: RAAS’s Impact on Filtration
GFR, or glomerular filtration rate, measures the kidneys’ ability to filter waste products from the blood. RAAS has a direct influence on GFR. Angiotensin II constricts the efferent arteriole, the blood vessel carrying blood away from the glomerulus. This constriction increases the pressure within the glomerulus, promoting GFR and enhancing filtration.
Maintaining the Balance: A Harmonious Partnership
RAAS works hand in hand with the kidneys to ensure a constant, optimal blood volume and blood pressure. When blood volume falls, RAAS activates its domino effect, leading to increased sodium reabsorption, elevated blood pressure, and enhanced GFR. This symphony of hormonal signals helps restore balance.
Clinical Significance: A Therapeutic Target
Understanding RAAS has profound clinical implications. Many cardiovascular medications, such as ACE inhibitors and angiotensin II receptor blockers (ARBs) target RAAS to lower blood pressure and protect the kidneys from damage.
The Renin-Angiotensin-Aldosterone System, like an invisible guardian, works tirelessly to maintain our blood volume and blood pressure. Its intricate dance with the kidneys ensures the proper functioning of our cardiovascular system and overall health. By appreciating its crucial role, we acknowledge the importance of supporting this system for a life in balance.