Understanding Pathogen Exit Portals For Effective Infection Control
The second link in the chain of transmission is the portal of exit, which is the pathway through which pathogens leave the reservoir. It can be the respiratory, urinary, or digestive tract, or any other opening in the body. The choice of portal of exit influences the mode of transmission, which determines how the pathogen spreads from the reservoir to a susceptible host.
Understanding the Chain of Transmission: The Second Link to Disease Prevention
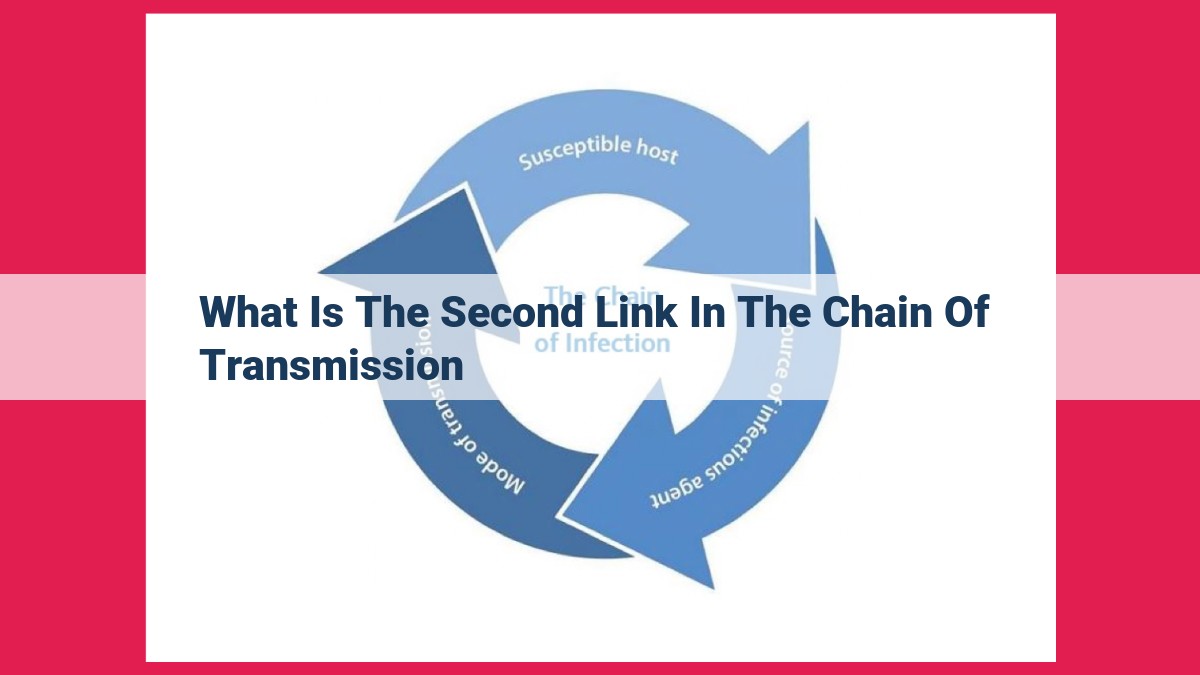
In the realm of disease control, understanding the chain of transmission is paramount. It’s a crucial concept that helps us trace the journey of infectious agents from their origin to a susceptible host. This chain consists of several interconnected links, and focusing on the second link – the portal of exit – is essential for effective prevention strategies.
Every disease begins with a reservoir, a haven where infectious agents reside and multiply. These reservoirs can be infected individuals, animals, or even contaminated objects. From the reservoir, pathogens must find a portal of exit to escape and infect others.
The portal of exit is the pathway through which pathogens exit their host. This could be the respiratory tract (e.g., coughing, sneezing), the urinary tract (e.g., excretion), or other bodily fluids. The choice of portal of exit influences the mode of transmission, the manner in which pathogens are transferred from one host to another.
Unveiling the **Second Link** in the Chain of Disease Transmission: The Portal of Exit
In understanding the intricate mechanisms of disease transmission, it’s essential to explore the concept of the chain of transmission. The second link in this chain, known as the portal of exit, plays a pivotal role in determining how pathogens spread from infected individuals or reservoirs to susceptible hosts.
The portal of exit serves as the gateway for pathogens to exit their host, paving the way for their transmission to new individuals. Various portals of exit exist, each offering a unique pathway for pathogens to escape. The respiratory tract is a common portal of exit, allowing pathogens to be expelled through coughing, sneezing, or talking. The urinary tract serves as another portal of exit, facilitating the release of pathogens through urine. Other portals of exit include the gastrointestinal tract, skin, and genital tract.
The choice of portal of exit significantly influences the mode of transmission, which refers to the specific pathway by which pathogens are transmitted to a new host. For instance, if pathogens exit through the respiratory tract, they can be transmitted through airborne transmission. When pathogens leave the host via the urinary tract, they can be transmitted through contact with contaminated surfaces or objects, such as doorknobs or bathroom fixtures.
By understanding the second link in the chain of transmission, public health officials can develop targeted strategies to prevent the spread of infection. Intervening at the portal of exit can disrupt the transmission cycle, effectively reducing the risk of disease spread. For example, respiratory hygiene practices, such as covering the mouth and nose when coughing or sneezing, help contain pathogens within the respiratory tract and prevent their expulsion into the environment. Hand hygiene, on the other hand, plays a crucial role in preventing the transmission of pathogens through contact with contaminated surfaces.
In summary, the portal of exit serves as a critical second link in the chain of disease transmission. Its influence on the mode of transmission highlights the importance of understanding the specific pathways by which pathogens escape from infected hosts. By targeting the portal of exit through effective control measures, we can effectively break the chain of transmission and protect individuals from the spread of infectious diseases.
Reservoirs and Their Impact on Disease Transmission
In the intricate web of disease transmission, reservoirs play a crucial role in sustaining and spreading pathogens. These reservoirs can be infected individuals, animals, or even contaminated objects. Imagine a hidden sanctuary where pathogens can thrive and multiply, waiting for the opportune moment to emerge and wreak havoc.
Infected Individuals as Reservoirs:
Humans are often the primary reservoirs for pathogens that cause diseases such as influenza and measles. Infected individuals harbor the pathogen within their body, providing a breeding ground for its replication. Their bodily fluids, such as respiratory droplets or blood, serve as potential exit portals for the pathogen to infect others. Understanding the behavior and infectious period of infected individuals is essential for effective disease control measures.
Animals as Reservoirs:
Animals can also act as reservoirs for certain pathogens. Consider the case of rabies, which is primarily transmitted through the saliva of infected animals, such as dogs, bats, or raccoons. Animals can carry the virus without showing symptoms, but their interactions with humans or other animals can lead to transmission. Recognizing the role of animals as reservoirs is crucial for preventing zoonotic diseases, which spread from animals to humans.
Contaminated Objects as Reservoirs:
Inanimate objects, such as contaminated surfaces or medical devices, can also harbor pathogens for extended periods. These objects can become reservoirs, facilitating the spread of infections in healthcare settings or public places. For example, methicillin-resistant Staphylococcus aureus (MRSA) can survive on surfaces for days, increasing the risk of transmission in hospitals. Identifying and disinfecting contaminated objects is vital for preventing infections from spreading through this pathway.
Factors Contributing to Pathogen Survival and Multiplication in Reservoirs:
The ability of a reservoir to sustain pathogens depends on several factors:
- Immune Status: The immune system of the reservoir can influence the survival and multiplication of pathogens. Immunocompromised individuals, such as those with HIV/AIDS or undergoing chemotherapy, are more likely to serve as reservoirs due to their weakened immune defenses.
- Environmental Conditions: Temperature, humidity, and pH levels can impact the survival of pathogens in reservoirs. For example, certain pathogens thrive in warm, humid environments, while others can withstand extreme cold or dryness. Understanding these environmental factors is essential for developing targeted control measures.
- Pathogen Characteristics: The ability of a pathogen to survive outside its host and establish itself in a reservoir depends on its characteristics, such as its ability to form spores or persist in dormant states.
By understanding the role of reservoirs in disease transmission, public health officials and healthcare professionals can develop strategies to break the chain of infection. Targeting the portal of exit and implementing measures to prevent pathogen survival and multiplication in reservoirs are crucial for controlling the spread of infectious diseases.
Understanding the Mode of Transmission
In the intricate dance of disease transmission, understanding its mode is key. The mode of transmission refers to the pathway by which a pathogen travels from its reservoir to infect a new host. This enigmatic journey unfolds through various portals, each with its unique mode of transmission.
Airborne Transmission:
If a pathogen’s portal of exit is the respiratory tract, it can hitch a ride on respiratory droplets, tiny particles expelled during coughing, sneezing, or even talking. These droplets can travel through the air, potentially infecting anyone who inhales them. Diseases like influenza and COVID-19 spread this way.
Contact Transmission:
When the portal of exit is the skin or mucous membranes, direct contact with an infected person or contaminated surfaces can lead to transmission. Examples include skin infections like scabies and sexually transmitted infections like HIV.
Indirect Contact Transmission:
Pathogens can also lurk on inanimate objects, known as fomites. When you touch or handle these contaminated surfaces, the pathogen may transfer to your hands and eventually enter your body. This mode is common for gastrointestinal infections like E. coli and norovirus.
Vector-Borne Transmission:
In nature’s intricate web, some pathogens enlist the services of tiny vectors like mosquitoes, ticks, or fleas. These vectors become infected by feeding on an infected host and can then transmit the pathogen to a new host during a subsequent bite. Examples include malaria, Lyme disease, and dengue fever.
The mode of transmission not only influences how pathogens spread but also guides our strategies for prevention and control. By targeting specific portals of exit and blocking the pathways of transmission, we can effectively combat disease outbreaks and protect public health.
**Implications for Disease Control: The Power of Understanding the Second Link**
The chain of transmission is a critical concept in disease control, providing a roadmap for understanding how infectious diseases spread. Understanding the second link in this chain, the portal of exit, is pivotal for developing effective strategies to prevent the spread of infections.
The portal of exit is the pathway through which pathogens, the disease-causing microorganisms, leave the infected host. By targeting the portal of exit, we can disrupt the chain of transmission and significantly reduce the risk of disease spread.
Respiratory Hygiene: Controlling Airborne Transmission
The respiratory tract is a common portal of exit for many viruses and bacteria. Infectious particles are released into the air through coughing, sneezing, or even talking, posing a risk of airborne transmission. Respiratory hygiene measures, such as covering coughs and sneezes with a tissue or elbow, and disposing of used tissues properly, effectively minimize the release of pathogens into the environment, reducing the risk of airborne transmission.
Hand Hygiene: Preventing Contact Transmission
Contact transmission occurs when pathogens are transferred through direct or indirect contact with infected materials. This includes touching contaminated surfaces, objects, or bodily fluids. Hand hygiene, particularly washing hands with soap and water or using alcohol-based hand sanitizers, is crucial for interrupting contact transmission. By removing pathogens from our hands, we prevent them from being transmitted to ourselves or others.
Vector Control: Blocking Intermediate Hosts
Certain diseases are transmitted through vectors, such as mosquitoes or ticks. These vectors serve as intermediate hosts for pathogens, which they acquire from infected hosts and transmit to new hosts. Vector control measures, such as mosquito nets, insect repellents, and eliminating breeding habitats, disrupt the transmission cycle and reduce the risk of vector-borne diseases.
Understanding the Second Link: A Key to Disease Prevention
By understanding the significance of the second link in the chain of transmission, we gain a powerful tool for preventing the spread of infections. Targeting the portal of exit allows us to develop and implement targeted interventions that effectively break the chain of transmission and protect public health. Respiratory hygiene, hand hygiene, vector control, and other measures based on this understanding are essential for creating a healthier, disease-free society.