Parathyroid Hormone Secretion: Regulation By Calcium Homeostasis And Essential Nutrients
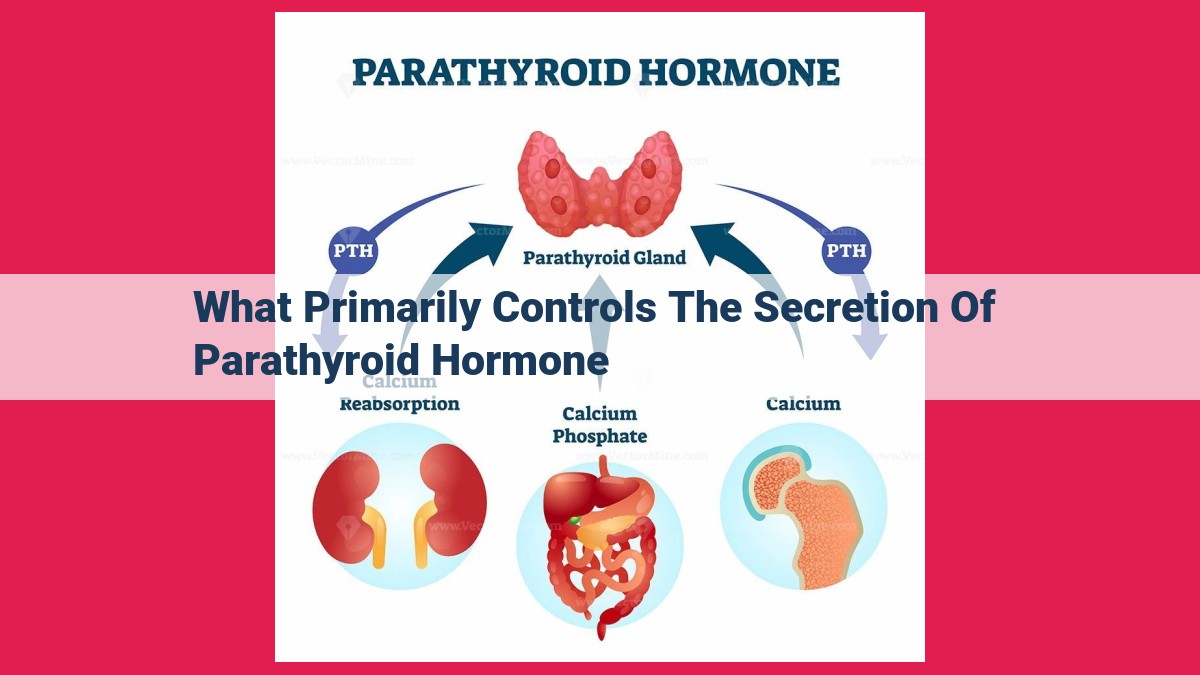
Parathyroid hormone (PTH) secretion is primarily controlled by calcium homeostasis. Low calcium levels trigger PTH release, which increases bone breakdown and renal reabsorption to restore calcium. Vitamin D suppresses PTH secretion through calcitriol, which promotes calcium absorption and bone mineralization. Calcitriol also modulates PTH secretion and calcium homeostasis. Magnesium and phosphorus levels also influence PTH secretion and calcium balance.
Calcium Homeostasis: The Primary Regulator of PTH Secretion
- Discuss the role of calcium levels in triggering PTH release.
- Explain how PTH increases calcium levels through bone breakdown and renal reabsorption.
Calcium Homeostasis: The Primary Regulator of PTH Secretion
Calcium, an essential mineral, plays a vital role in various bodily functions, including bone health, muscle contraction, and nerve transmission. Its levels in the bloodstream are meticulously regulated by a hormone called parathyroid hormone (PTH).
When calcium levels drop (hypocalcemia), the parathyroid glands sense the deficiency and respond by secreting PTH to raise calcium levels. PTH acts on bones, promoting the breakdown of bone tissue to release calcium into the bloodstream. This process, known as bone resorption, is crucial for maintaining adequate calcium levels in the face of low dietary intake or increased calcium demand.
PTH also targets the kidneys, enhancing calcium reabsorption from urine back into the blood. By promoting bone breakdown and increasing renal reabsorption, PTH effectively elevates calcium levels towards normal. This regulatory mechanism ensures the availability of calcium for essential physiological processes, such as muscle function, nerve conduction, and proper bone mineralization.
Vitamin D: Inhibiting PTH Secretion for Calcium Homeostasis
Vitamin D plays a crucial role in maintaining our calcium balance, influencing parathyroid hormone (PTH) secretion. This sunlight vitamin undergoes a remarkable transformation in our bodies, converting to calcitriol, its active form.
Calcitriol emerges as a suppressor of PTH secretion. As vitamin D levels rise, so does calcitriol production, which signals to our parathyroid glands to reduce PTH release. This intricate interplay is essential for regulating calcium levels in our blood.
When calcium levels drop, PTH secretion increases, prompting our bodies to release calcium from bone stores and enhance its reabsorption from the kidneys. However, when vitamin D levels are abundant, calcitriol steps in to curb PTH production, preventing excessive calcium release and maintaining a healthy equilibrium.
Furthermore, calcitriol directly influences calcium metabolism. It promotes calcium absorption in our intestines, ensuring an adequate supply for our bones and other bodily functions. Additionally, calcitriol enhances bone mineralization, ensuring strong and healthy skeletal structures.
In summary, vitamin D and its active metabolite, calcitriol, play a vital role in regulating PTH secretion and maintaining calcium homeostasis. By suppressing PTH production and promoting calcium absorption and bone mineralization, these nutrients work in harmony to ensure optimal calcium levels for our overall well-being.
Calcitriol: A Modulator of PTH Secretion and Calcium Homeostasis
Calcitriol, the active form of vitamin D, plays a crucial role in calcium metabolism and bone health. It works in concert with parathyroid hormone (PTH) to ensure that calcium levels in the body are maintained within a narrow range.
Role of Calcitriol in Promoting Calcium Absorption and Bone Mineralization
Calcitriol’s primary function is to promote the absorption of calcium from the intestines. It does this by increasing the expression of calcium-binding proteins in the intestinal lining, which facilitates the uptake of calcium ions.
In addition to enhancing calcium absorption, calcitriol also promotes bone mineralization. It stimulates the production of osteoblasts, the cells responsible for building new bone tissue. Calcitriol also increases the deposition of calcium and phosphate ions into the bone matrix, making bones stronger and more resilient.
Calcitriol’s Influence on PTH Secretion and Calcium Homeostasis
The interplay between calcitriol and PTH is essential for maintaining calcium homeostasis. When calcium levels in the blood drop, the parathyroid glands release PTH. PTH then stimulates the release of calcitriol from the kidneys.
Calcitriol acts on several target tissues to increase calcium levels in the blood. It promotes calcium absorption in the intestines and reabsorption in the kidneys. Calcitriol also inhibits the expression of PTH in the parathyroid glands, reducing its secretion. This negative feedback loop helps to keep calcium levels within a normal range.
In summary, calcitriol plays a multifaceted role in calcium homeostasis. It promotes calcium absorption, enhances bone mineralization, and modulates PTH secretion. By working in conjunction with PTH, calcitriol ensures that the body has the calcium it needs to maintain healthy bones and support a variety of physiological functions.
Magnesium: A Balancing Act for Parathyroid Hormone Secretion
In the intricate dance of calcium homeostasis, magnesium emerges as an unsung hero, subtly influencing the symphony of hormonal interplay. Magnesium, an essential mineral, weaves its way through the tapestry of bone metabolism and neuromuscular harmony.
Bone’s Silent Guardian: Magnesium’s presence in bone tissue is crucial, playing a vital role in crystal formation, strengthening our skeletal framework. It acts as a gatekeeper, ensuring that calcium ions find their proper place within bone, promoting mineralization and preventing fragile bones.
Neuromuscular Equilibrium: Beyond its skeletal contributions, magnesium plays a pivotal role in neuromuscular function. It serves as a cofactor, enabling enzymes involved in nerve impulse transmission and muscle contraction. Without adequate magnesium, our nerves and muscles may falter, leading to tremors, muscle cramps, and a weakened grip on our everyday movements.
Magnesium’s Influence on PTH: Magnesium’s impact on parathyroid hormone (PTH) secretion, the master regulator of calcium homeostasis, is indirect but profound. When magnesium levels dip, PTH secretion rises, as if the body is trying to compensate for the potential calcium imbalance.
Impact on Calcium Balance: The increased PTH levels elevate calcium levels by promoting bone breakdown and enhancing renal reabsorption of calcium. This counteracts the loss of calcium that would otherwise occur due to magnesium deficiency.
Conclusion: Magnesium, though often overlooked, is an indispensable player in the orchestration of calcium homeostasis. Its presence ensures strong bones, steady nerves, and the delicate balance that allows us to move, function, and thrive. Understanding magnesium’s influence on PTH secretion highlights its multifaceted role in maintaining our overall well-being.
Phosphorus: A Delicate Balance in PTH Secretion
Phosphorus, a crucial mineral, plays a multifaceted role in our bodies, contributing to the strong foundation of our bones and the efficient production of energy. It’s a dance that balances bone metabolism and energy efficiency, delicately influencing the secretion of parathyroid hormone (PTH).
Phosphorus’s Vital Role in Bone Health and Energy Production
As a primary component of bones, phosphorus plays an indispensable part in their rigidity and strength. Adequate phosphorus levels ensure that our bones can bear weight and support movement. Moreover, phosphorus serves as a critical element in energy production. It participates in the creation of ATP, the energy currency of our cells, enabling us to perform everyday tasks and power our bodily functions.
The Dueling Effects of Phosphorus on PTH Secretion
The body maintains phosphorus levels within a narrow range, and any deviation from this range can disrupt PTH secretion and calcium homeostasis. Hyperphosphatemia, or high phosphate levels, inhibits PTH secretion. This suppression stems from a feedback mechanism where elevated phosphate levels reduce the sensitivity of the parathyroid glands to low calcium levels. As a result, PTH production decreases.
Conversely, hypophosphatemia, or low phosphate levels, stimulates PTH secretion. A lack of phosphate triggers a compensatory response in the body, where increased PTH production aims to boost renal phosphate reabsorption and bone resorption, thereby raising phosphate levels.
The Dance of PTH and Phosphorus in Calcium Homeostasis
PTH plays a pivotal role in regulating calcium levels in our blood. It stimulates bone breakdown to release calcium, promoting an increase in blood calcium levels. Simultaneously, PTH enhances calcium reabsorption in the kidneys, further elevating calcium levels.
Phosphorus, as a partner in this dance, exerts its influence on PTH secretion and, consequently, calcium homeostasis. High phosphate levels suppress PTH production, leading to a decline in calcium release from bones and decreased renal calcium reabsorption. Conversely, low phosphate levels stimulate PTH release, enhancing calcium release from bones and increasing renal calcium reabsorption.
Thus, phosphorus, with its ability to influence PTH secretion, stands as a crucial player in maintaining the delicate balance of calcium homeostasis, ensuring the proper functioning of our bodies and the health of our bones.