Kirby-Bauer Test: Accurately Assessing Bacterial Susceptibility For Optimal Antibiotic Selection
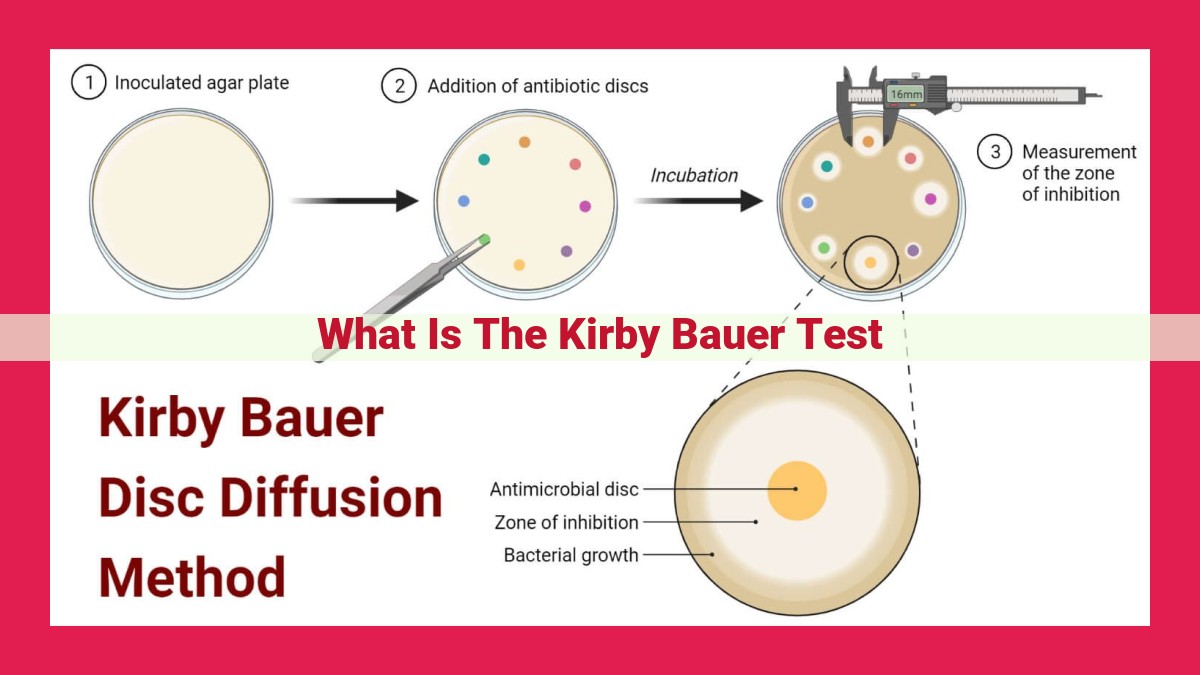
The Kirby-Bauer Test, an antibiotic susceptibility testing method, assesses bacterial susceptibility by measuring the size of inhibition zones formed around antibiotic-impregnated discs placed on an agar plate inoculated with bacterial growth. Zones indicate susceptibility (large zone), intermediate susceptibility (medium zone), or resistance (small or no zone). This test aids in determining appropriate antibiotic choices for targeted therapy, guiding optimal treatment decisions and preventing antimicrobial resistance.
- Introduce the Kirby-Bauer Test as an antibiotic susceptibility testing method.
- Discuss its significance in identifying effective antibiotics.
Antibiotic Susceptibility Testing: Unveiling the Kirby-Bauer Test
In the relentless battle against infectious diseases, antibiotics have emerged as our formidable allies. However, the emergence of antimicrobial resistance demands a dynamic approach to identify the most effective antibiotics for each patient. Enter the Kirby-Bauer Test, a cornerstone of antibiotic susceptibility testing.
This ingenious test harnesses the power of diffusion to determine an antimicrobial’s potency against specific bacteria. By pitting bacteria against an array of antibiotics on an agar plate, we can witness their tug-of-war: the antibiotics diffusing outward, valiantly attempting to subdue the bacterial invaders.
Witnessing the Battle: The Diffusion Method
The Kirby-Bauer Test is an elegant dance of precision. A bacterial culture is meticulously spread onto an agar plate, creating a uniform canvas for the antibiotic discs to alight. These discs, impregnated with known antibiotic concentrations, are then gently placed on the plate, akin to warriors awaiting the battle’s commencement.
As the plate incubates, a mesmerizing spectacle unfolds. The antibiotics, eager to fulfill their duty, diffuse outward in concentric circles. If an antibiotic has the prowess to vanquish the bacteria, a distinct zone of inhibition emerges around the disc—a clear testament to its potency.
Decoding the Zones: A Tale of Susceptibility
The size of the zone of inhibition is a teller of tales, narrating the susceptibility of the bacteria to the antibiotic. A larger zone indicates a formidable foe, effectively inhibiting the bacteria’s growth. Conversely, a smaller zone signals a weaker opponent, allowing the bacteria to persist.
This crucial information empowers clinicians to tailor antibiotic therapy, selecting the most potent weapon to combat the specific bacteria causing the infection. It guides them in determining the appropriate antibiotic, dosage, and duration of treatment, ultimately optimizing patient outcomes.
A Sentry against Antimicrobial Resistance
The Kirby-Bauer Test also plays a pivotal role in the surveillance and prevention of antimicrobial resistance. By monitoring antibiotic susceptibility patterns, we can identify resistant strains that are becoming increasingly prevalent in our communities.
A Beacon in the Clinical Arena
The Kirby-Bauer Test is a cornerstone in the clinical arena, providing invaluable insights into antibiotic susceptibility. It ensures the judicious use of antibiotics, preventing the development of antimicrobial resistance and safeguarding the efficacy of these vital medications.
Diffusion Method in the Kirby-Bauer Test: The Journey of Antibiotic Susceptibility
Imagine a world where infections run rampant, and antibiotics are our only defense. To ensure these precious weapons remain effective, we rely on antibiotic susceptibility testing, and one of the most trusted methods is the Kirby-Bauer Test.
At the heart of this test lies the diffusion method. Like a culinary experiment, we start with preparing our ingredients:
-
Bacterial Inoculum: Our target, the bacteria, is carefully spread onto an agar plate, creating a uniform lawn of microbial life. This lawn becomes the battlefield where the antibiotic discs will wage their war.
-
Antibiotic Discs: These small paper rounds are saturated with precise concentrations of specific antibiotics. They represent the weapons we’ll deploy against the bacteria.
Once our ingredients are ready, the incubation begins. The agar plate, a petri dish of sorts, is placed in a warm, cozy environment, and the battle lines are drawn.
Diffusion takes center stage as the antibiotics slowly spread outward from their discs, creating a zone of inhibition. Like ripples in a pond, these zones are a testament to the antibiotic’s ability to quell the bacterial growth. Their size, measured with calipers, holds the key to determining the bacteria’s susceptibility.
The larger the zone of inhibition, the more potent the antibiotic’s effect against the bacteria. This information empowers healthcare professionals to make informed decisions about the most appropriate antibiotic choices and dosages for specific infections.
In the grand scheme of combating infections and preventing antimicrobial resistance, the Kirby-Bauer Test plays a vital role. By identifying effective antibiotics, it ensures that patients receive the optimal treatment, improving outcomes and preserving the effectiveness of our invaluable antibiotic arsenal.
The Critical Role of Antibiotic Discs in the Kirby-Bauer Test
In the realm of battling bacterial infections, the Kirby-Bauer Test emerges as a vital tool, providing invaluable information about which antibiotics can effectively halt the microbial aggressors. This test relies heavily upon Antibiotic Discs, small yet powerful tools that play a critical role in assessing bacterial susceptibility.
Types and Concentrations of Antibiotics
Antibiotic Discs contain various types and concentrations of antibiotics, each tailored to target specific bacteria. These discs are meticulously selected to represent a broad spectrum of antimicrobial agents. The choice of antibiotics depends on the suspected infection and the patient’s medical history. By exposing bacteria to a range of antibiotics, the Kirby-Bauer Test can determine which ones can inhibit or kill the bacteria effectively.
Placement and Significance
Once the antibiotic discs are chosen, they are carefully placed on an agar plate containing the bacterial sample. Each disc is equidistant from the others, ensuring consistent diffusion of the antibiotics into the agar. The placement of the discs is crucial as it allows for clear and distinct zones of inhibition to form around the discs.
Zones of Inhibition
As the antibiotics diffuse through the agar, they create circular zones of inhibition, areas where bacterial growth is suppressed. The size of these zones is directly proportional to the susceptibility of the bacteria to the antibiotic. Larger zones indicate greater susceptibility, while smaller zones suggest resistance. By measuring the zones of inhibition and comparing them to standardized breakpoints, clinicians can determine the susceptibility of the bacteria to each antibiotic.
Antibiotic Discs are indispensable components of the Kirby-Bauer Test, providing a standardized method for assessing bacterial susceptibility to antibiotics. Their careful selection, placement, and interpretation allow clinicians to make informed decisions about antibiotic therapy, ensuring optimal patient outcomes and combating the growing threat of antimicrobial resistance.
Zone of Inhibition Measurement and Interpretation: Unraveling Bacterial Susceptibility
The Kirby-Bauer Test, a cornerstone of antibiotic susceptibility testing, employs the diffusion method to assess how bacteria respond to antibiotics. This involves placing antibiotic-impregnated discs onto an agar plate seeded with the target bacteria. As the antibiotics diffuse outward from the discs, they create zones of inhibition where bacterial growth is prevented.
The size of these zones is a crucial indicator of bacterial susceptibility. Larger zones represent greater susceptibility, as the antibiotic is effectively inhibiting bacterial growth. Conversely, smaller zones or complete absence of zones indicate resistance or reduced susceptibility, as the bacteria are able to withstand the antibiotic.
Measuring Zones of Inhibition
Precise measurement of zone diameters is essential for accurate interpretation. Using a calibrated ruler or caliper, the distance from the edge of the antibiotic disc to the clear zone boundary is measured in millimeters. It’s important to exclude any hazy area of partial inhibition, as this may indicate reduced susceptibility.
Correlation with Bacterial Susceptibility
Zone size is directly correlated with bacterial susceptibility. The larger the zone, the more susceptible the bacteria are to the antibiotic. This relationship is standardized through breakpoints, which are established criteria for defining susceptibility, intermediate susceptibility, and resistance. These breakpoints are specific to each antibiotic-bacteria combination and are regularly updated based on research and clinical data.
Minimum Inhibitory Concentration (MIC): The Key to Unlocking Antibiotic Efficacy
The Kirby-Bauer Test is an essential tool in the fight against bacterial infections. It provides valuable information about which antibiotics are most effective against a particular bacterial strain. One key aspect of this test is the determination of Minimum Inhibitory Concentration (MIC) values.
MIC is the lowest concentration of an antibiotic that can completely inhibit the growth of a specific bacterium. It’s a crucial metric because it directly correlates with the susceptibility of the bacterium to that antibiotic.
The MIC is typically determined through a series of dilution tests. A range of antibiotic concentrations are prepared and inoculated with the target bacterium. After incubation, the lowest concentration at which no bacterial growth is observed is determined to be the MIC.
The MIC value provides additional information beyond the zone of inhibition observed in the Kirby-Bauer Test. While the zone of inhibition gives a general indication of susceptibility, the MIC provides a precise measurement of the antibiotic’s effectiveness.
Understanding the MIC is critical for the optimal management of bacterial infections. It helps clinicians determine the appropriate dosage of an antibiotic and can detect emerging antimicrobial resistance. By identifying the MIC, healthcare professionals can optimize antibiotic therapy, ensuring effective treatment and minimizing resistance development.
Interpreting Kirby-Bauer Test Results: Unveiling Bacterial Susceptibility
The Kirby-Bauer Test is a vital tool that aids in determining antibiotic susceptibility, a crucial aspect in combating bacterial infections effectively. Interpreting the test results involves categorizing bacterial responses into three distinct groups: susceptible, intermediate, and resistant.
Susceptible: When bacteria demonstrate sensitivity to a specific antibiotic, they are deemed susceptible. The test result shows zones of inhibition with a diameter larger than the established breakpoints.
Intermediate: This category indicates partial susceptibility, where bacteria demonstrate some resistance but remain vulnerable to higher antibiotic concentrations. The zone of inhibition for bacteria in this category falls within the established breakpoint range.
Resistant: Bacteria that are resistant to an antibiotic exhibit strong resistance and require higher concentrations to inhibit their growth. The zone of inhibition for resistant bacteria is smaller than the established breakpoint.
Breakpoints: Guiding the Interpretation
Breakpoints, threshold values, serve as critical guidelines in defining the susceptibility categories. These values are established through standardized testing and reflect the minimum antibiotic concentration required to inhibit the growth of specific bacteria.
Accurate Reporting for Optimal Outcomes
Accurate interpretation of Kirby-Bauer Test results is crucial for optimizing patient outcomes. It ensures that patients receive appropriate antibiotic therapy, aiding in:
- Effectively combating infections
- Preventing unnecessary antibiotic use
- Minimizing the development of antimicrobial resistance
Antimicrobial Resistance Monitoring: The Critical Role of the Kirby-Bauer Test
Antimicrobial resistance poses a serious threat to global public health, undermining the effectiveness of antibiotics and making once-treatable infections deadly. The Kirby-Bauer Test stands as a crucial tool in monitoring these evolving resistance patterns, safeguarding patients against inappropriate antibiotic use and ensuring optimal treatment outcomes.
- Mechanisms of Antimicrobial Resistance:
Bacteria have developed ingenious mechanisms to evade the effects of antibiotics. Some produce enzymes that break down antibiotics, while others alter their target sites or create impenetrable barriers. Understanding these resistance mechanisms is essential for developing new drugs and strategies to combat them.
- The Role of the Kirby-Bauer Test:
The Kirby-Bauer Test plays a pivotal role in monitoring antimicrobial resistance. It reveals the susceptibility of bacteria to various antibiotics, identifying strains that have developed resistance. By comparing the size of inhibition zones around antibiotic discs on agar plates, laboratories can assess the effectiveness of different drugs against specific bacterial isolates.
This information is critical for guiding antibiotic therapy and preventing the spread of resistant bacteria. By identifying resistant strains, clinicians can tailor treatments to non-resistant antibiotics, minimizing the selection pressure that fuels resistance development.
The Kirby-Bauer Test is an invaluable tool in the fight against antimicrobial resistance. It provides in-depth information on bacterial susceptibility patterns, enabling clinicians to make informed decisions about antibiotic therapy. Its continued use will help ensure that antibiotics remain effective and that patients receive the best possible treatment.
Clinical Significance of the Kirby-Bauer Test: A Guiding Light in Antibiotic Therapy
The Kirby-Bauer Test is an invaluable tool in the medical arsenal, providing crucial information that guides antibiotic therapy for optimal patient outcomes. By determining the susceptibility of bacteria to various antibiotics, this test empowers healthcare professionals to make informed decisions about the most effective treatment options.
Identifying the Right Antibiotics
The Kirby-Bauer Test helps identify antibiotics that can effectively combat infection-causing bacteria. It reveals the bacteria’s susceptibility profile, indicating which antibiotics they are sensitive or resistant to. This knowledge is vital in choosing the most appropriate antibiotic, ensuring targeted therapy that maximizes efficacy and minimizes side effects.
Optimizing Dosage and Duration
The test also provides guidance on the appropriate dosage and duration of antibiotic therapy. By correlating the zone of inhibition with the minimum inhibitory concentration (MIC), clinicians can determine the optimal antibiotic concentration needed to effectively treat the infection. This personalized approach reduces the risk of underdosing, which can lead to treatment failure, and overdosing, which can cause unnecessary adverse effects.
Combating Antimicrobial Resistance
The Kirby-Bauer Test plays a critical role in the fight against antimicrobial resistance, a growing global health concern. It allows healthcare providers to monitor resistance patterns in bacteria, enabling targeted interventions to prevent the spread of resistant strains. By identifying resistant bacteria early on, the test helps optimize antibiotic use, reducing the risk of future infections that are more difficult to treat.
Empowering healthcare professionals with essential information, the Kirby-Bauer Test is a cornerstone of effective antibiotic therapy. It guides the selection of appropriate antibiotics, optimizes dosage and duration, and contributes to the fight against antimicrobial resistance. By leveraging this powerful tool, clinicians are better equipped to provide the best possible care and improve patient outcomes.
Laboratory Protocol: A Comprehensive Guide to Performing the Kirby-Bauer Test
The Kirby-Bauer Test is an essential antibiotic susceptibility testing method that plays a vital role in guiding appropriate antibiotic therapy. This step-by-step protocol will provide a detailed understanding of how to perform the test effectively, including quality control measures and standardization practices.
Materials and Equipment
- Bacterial isolate
- Mueller-Hinton agar plates
- Antibiotic discs
- Sterile cotton swabs
- Sterile saline or broth
- Calipers or ruler
- Incubator
- Quality control strains
Procedure
-
Prepare Bacterial Inoculum: Suspend the bacterial isolate in sterile saline or broth to achieve a specific turbidity (0.5 McFarland standard).
-
Inoculate Agar Plates: Dip a sterile cotton swab into the bacterial suspension and gently swab the entire surface of a Mueller-Hinton agar plate.
-
Apply Antibiotic Discs: Using sterile forceps, place the antibiotic discs onto the inoculated agar plate at predetermined distances.
-
Incubate: Incubate the plates at 35-37°C for 16-18 hours.
-
Measure Zones of Inhibition: After incubation, measure the zones of inhibition surrounding each antibiotic disc using calipers or a ruler.
Quality Control and Standardization
-
Quality control strains: Test known strains with susceptible, intermediate, and resistant profiles to ensure the accuracy of the test.
-
Standardization: Follow standardized procedures, including the use of calibrated equipment and adherence to established guidelines, to ensure reproducible results.
Interpretation of Results
The zone of inhibition size corresponds to the susceptibility of the bacterial isolate to the specific antibiotic. Breakpoints are used to categorize the isolates as susceptible, intermediate, or resistant.
Monitoring Antimicrobial Resistance
The Kirby-Bauer Test is crucial for monitoring antimicrobial resistance patterns. By tracking changes in antibiotic susceptibility over time, healthcare professionals can identify emerging resistance mechanisms and implement strategies to combat them.
Clinical Significance
The Kirby-Bauer Test is a fundamental tool in guiding antibiotic therapy. By identifying appropriate antibiotic choices and dosages, it helps optimize patient outcomes and prevent the development of antimicrobial resistance.