Host Susceptibility To Pathogens: Exploring The Interplay Of Virulence, Defenses, And Zoonotic Interactions
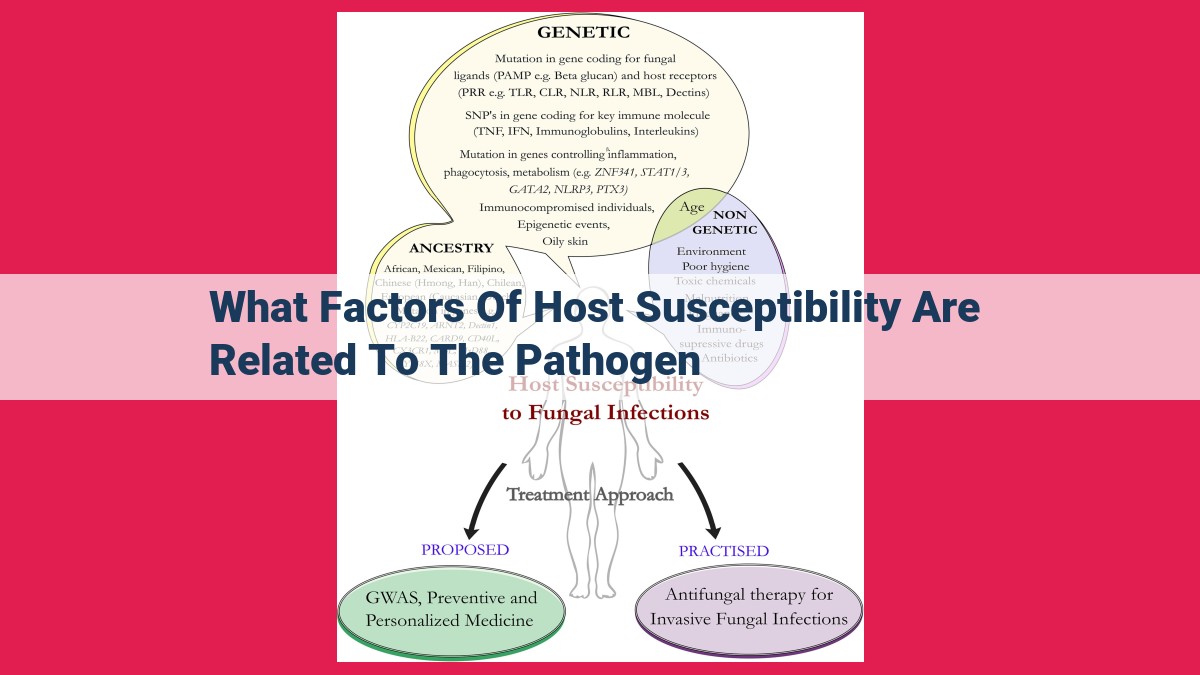
Host susceptibility to pathogens is influenced by factors related to the pathogen’s virulence, host defenses, and their interaction. Pathogen factors such as adhesion, invasion, replication, and pathogenicity contribute to disease severity. Host factors like immune function, genetic variations, and zoonotic exposures determine susceptibility to specific pathogens. Understanding these factors is crucial for developing targeted therapies and preventing disease outbreaks involving both vectors and animal reservoirs.
Factors of Host Susceptibility Related to Pathogens: A Comprehensive Guide
Pathogens, whether they be bacteria, viruses, or parasites, are constantly evolving to overcome the defenses of their hosts. Understanding the role of host factors in this battle is crucial for preventing and treating infectious diseases.
Host Factors in Disease Susceptibility
*Host factors* encompass a wide range of characteristics that influence an individual’s susceptibility to pathogens. These factors can be genetic, such as inherited differences in immune function, or acquired, such as the microbiome, nutrition, and lifestyle choices.
Host factors play a critical role in pathogenesis, the process by which pathogens cause disease. By understanding these factors, we can develop more effective strategies to protect individuals from infection and treat those who become sick.
Adhesion and Colonization
Pathogens must first adhere to and colonize the host in order to cause disease. Host factors such as mucosal barriers and immune responses play a significant role in preventing or promoting this process.
- Mucosal barriers, such as the lining of the respiratory and digestive tracts, provide a physical barrier against pathogens.
- Immune responses, such as the production of antibodies and the activation of immune cells, can recognize and eliminate pathogens that breach these barriers.
Invasion
Once pathogens have colonized the host, they may need to invade host cells to replicate and spread infection. Host factors such as immune deficiencies and cell signaling pathways can influence the efficiency of invasion.
- Immune deficiencies can weaken the host’s defenses against pathogens, making them more susceptible to invasion.
- Cell signaling pathways can regulate the production of proteins that facilitate or inhibit pathogen entry into host cells.
Replication
For pathogens to cause disease, they must replicate within the host. Host factors such as antibiotics and host defense mechanisms can inhibit bacterial replication and prevent infection from spreading.
- Antibiotics are drugs that specifically target bacterial cells, interfering with their replication and killing them.
- Host defense mechanisms, such as the production of antimicrobial peptides, can also inhibit bacterial replication and promote host recovery.
Factors of Host Susceptibility Related to Pathogens: A Comprehensive Guide
In the intricate dance between hosts and pathogens, host factors play a pivotal role in determining the susceptibility and severity of infectious diseases. These factors are like the stage on which the drama of infection unfolds, influencing every aspect of the pathogen’s journey.
Adhesion and Colonization
The initial encounter between a pathogen and its host is marked by the adhesion of the pathogen to the host’s surface. This seemingly simple act is orchestrated by intricate mechanisms, involving bacterial factors like adhesins that bind to specific receptors on host cells. These connections allow the pathogen to gain a foothold, establishing a biofilm, a protective community that enhances their survival and colonization.
Invasion
Once established, pathogens seek to penetrate the host’s defenses. They employ specialized virulence factors that enable them to invade host cells. This process can be aided by host immune responses or cell signaling pathways that inadvertently provide a gateway for the pathogen. In contrast, immune deficiencies or dysregulation can hinder the pathogen’s ability to breach the host’s defenses.
Replication
Within the host, the pathogen strives to replicate and proliferate. This process is influenced by the host’s antibiotic sensitivity and immune defense mechanisms. Antibiotics target bacterial processes, while the immune system’s arsenal of cells and molecules fights the invading pathogen. The outcome of this battle will determine the pathogen’s ability to establish a foothold and cause disease.
**The Enigmatic Dance of Bacteria and Host: A Tale of Adhesion and Colonization**
In the intricate web of life, pathogens and hosts engage in a delicate dance, where the outcome can spell the difference between health and disease. At the heart of this dynamic is bacterial adherence, a pivotal step that sets the stage for colonization and the potential for infection.
Bacteria, armed with an arsenal of clever strategies, employ specialized structures called adhesins to cling tenaciously to host cells. These adhesins, often proteins, act like molecular grappling hooks, latching onto specific receptors on the host’s surface. It’s a complex and finely tuned process, with different bacteria targeting different receptors on a variety of host cells.
Take, for instance, the notorious Streptococcus pneumoniae, the culprit behind pneumonia and other infections. It boasts a repertoire of adhesins that bind to receptors on the respiratory tract, allowing it to colonize and establish a foothold. Similarly, Escherichia coli, a common inhabitant of the gut, uses its fimbriae, hair-like projections, to adhere to receptors in the intestinal lining, ensuring its survival and potential to cause infections.
The host, however, is not a passive participant in this dance. Its own defenses come into play, including mucosal barriers that line vulnerable surfaces and immune responses that recognize and target foreign invaders. These defenses act as formidable gatekeepers, preventing bacteria from gaining access to deeper tissues and causing systemic infections.
In this intricate interplay, both the bacterium’s adhesins and the host’s defenses play a critical role in determining susceptibility to infection. By understanding these mechanisms, we gain valuable insights into the development of strategies to prevent and treat infectious diseases, safeguarding our health and well-being.
Describe the Formation of Biofilms and Their Impact on Colonization
Picture this: you’ve just had a minor cut on your finger. No big deal, right? But what happens when the wound becomes infected and starts to ooze? It could be due to biofilms, slimy, protective communities that bacteria form to shield themselves from threats.
How do these biofilms form? It’s a bit like a city. Bacteria adhere to surfaces, like your skin or a medical device, and then colonize, forming microcolonies. As they grow and multiply, they produce a sticky substance called extracellular polymeric substance (EPS), which forms a protective matrix around them. This matrix is like a fortress, defending the biofilm from antibiotics, the immune system, and other environmental threats.
The impact of biofilms on colonization is significant. They make it much harder for bacteria to be removed, which can lead to persistent infections. In the case of implants, for example, biofilms can cause infections that are difficult to treat and may require the implant to be removed. Biofilms also play a role in device-related infections, such as those associated with catheters and ventilators, and in chronic infections, such as those of the lungs or middle ear.
Understanding the role of biofilms in colonization is crucial for developing effective prevention and treatment strategies for bacterial infections. By targeting the formation, growth, and persistence of biofilms, we can improve patient outcomes and reduce the burden of disease.
How Mucosal Barriers and Immune Responses Protect Against Bacterial Adhesion
When pathogens attempt to invade our bodies, mucosal barriers serve as the front line of defense. These barriers consist of physical barriers, such as the skin and mucosal membranes, and chemical barriers, such as mucus and antimicrobial peptides. Together, they create a protective layer that prevents pathogens from directly contacting host cells and initiating an infection.
Mucosal membranes are especially important in preventing bacterial adhesion. They line various passages in the body, including the respiratory, digestive, and urogenital tracts. These membranes are composed of epithelial cells that secrete mucus, a thick, sticky substance that traps and expels foreign particles, including bacteria. The surface of epithelial cells also contains receptors that bind to specific antigens on the surface of bacteria, triggering immune responses.
If bacteria manage to penetrate the mucosal barrier, they face another formidable obstacle: the immune system. The immune system is a complex network of cells, proteins, and signaling molecules that recognizes and attacks pathogens. When bacteria adhere to host cells, they release toxins and enzymes that can damage the cells and promote colonization. In response, the immune system activates immune cells such as neutrophils and macrophages that phagocytose (ingest) the bacteria and release antimicrobial substances.
The mucosal immune system also plays a crucial role in preventing bacterial adhesion. It contains specialized immune cells called mucosal-associated lymphoid tissue (MALT) cells that are located within the mucosal membranes. MALT cells produce antibodies that recognize and neutralize bacteria, making them less likely to adhere to host cells.
Other host factors that influence bacterial adhesion include genetic variations, nutritional status, and stress levels. For example, mutations in genes that encode proteins involved in mucosal barrier function can increase susceptibility to bacterial infections. Poor nutrition can weaken the immune system, making it less effective at clearing bacteria. And chronic stress can suppress immune responses, increasing the risk of bacterial adhesion and colonization.
By understanding how host factors such as mucosal barriers and immune responses influence bacterial adhesion, we can develop new strategies to prevent and treat bacterial infections. These strategies could include strengthening mucosal defenses, enhancing immune responses, and targeting bacterial adherence mechanisms.
Explore the Mechanisms of Bacterial Entry into Host Cells: A Stealthy Invasion
Bacteria, the microscopic invaders, possess an array of strategies to breach the formidable defenses of host cells and establish their stronghold. Their entry into host cells is a critical step in the infectious process, shaping the severity and progression of the disease. Understanding these mechanisms is essential for developing effective therapeutic interventions.
One common mechanism employed by bacteria is direct invasion. Here, the bacteria physically penetrate the host cell membrane, often exploiting specific receptors on the surface. Some bacteria, such as Salmonella, have evolved sophisticated needle-like structures called type III secretion systems. These systems act like tiny spears, injecting bacterial proteins into the host cell and facilitating entry.
In other cases, bacteria use more subtle strategies to gain access. Some bacteria, like Mycobacterium tuberculosis, hijack the host cell’s own endocytic pathways. By mimicking host molecules, they trick the cell into engulfing them through processes such as phagocytosis or pinocytosis.
Once inside the host cell, the bacteria face a new set of challenges. They must navigate the complex cellular environment, evade detection by the immune system, and find a suitable niche to replicate and thrive. The ability of bacteria to adapt and overcome these challenges highlights their remarkable resilience and the importance of understanding the mechanisms of their entry into host cells.
By deciphering these strategies, scientists can identify potential targets for new antibiotics and treatments. This knowledge can lead to the development of therapies that disrupt bacterial entry, preventing the establishment of infection and improving patient outcomes.
**Factors of Host Susceptibility Related to Pathogens: A Comprehensive Outline**
- Host factors in disease susceptibility: Host factors play a crucial role in determining an individual’s susceptibility to pathogens.
- Pathogen-host interactions: Host factors influence the ability of pathogens to adhere, invade, replicate, and cause disease.
**2. Invasion**
- Bacterial entry into host cells: Pathogens employ various mechanisms to penetrate host cell membranes.
- Immune responses and cell signaling: The host immune system recognizes and responds to invading bacteria, triggering defense mechanisms that inhibit invasion.
- Host factors affecting invasion: Immune deficiencies and genetic variations can impact the effectiveness of bacterial invasion strategies.
How Host Immune Deficiencies Affect Bacterial Invasion Efficiency
The ability of bacteria to successfully invade host cells is a crucial step in establishing infection and causing disease. While the mechanisms of bacterial invasion vary, a common theme is the interaction between bacterial virulence factors and host immune responses. In this section, we will explore how host immune deficiencies can affect the efficiency of bacterial invasion, highlighting the importance of a robust immune system in preventing bacterial infections.
Immune Deficiencies: A Gateway for Bacterial Invasion
The immune system is a complex network of cells, tissues, and molecules that work together to defend the body against pathogens. Immune deficiencies, resulting from genetic defects, malnutrition, or disease, can impair the immune system’s ability to detect, identify, and eliminate bacterial invaders. These deficiencies can create a window of opportunity for bacteria to exploit and gain a foothold in the host.
Impaired phagocytosis, a process where immune cells engulf and destroy pathogens, is a significant immune deficiency that can increase susceptibility to bacterial infections. Phagocytes, such as macrophages and neutrophils, are critical for eliminating bacteria that have entered the body. However, defects in phagocytosis can result in the bacteria evading immune detection and establishing infection.
Another important immune response is the complement system, a group of proteins that enhance the ability of antibodies to neutralize and kill bacteria. Deficiencies in the complement system, such as the inability to produce certain complement proteins, can result in reduced bacterial killing and increased susceptibility to infection.
Role of Antibodies in Preventing Invasion
Antibodies are specialized proteins produced by the immune system to recognize and neutralize specific pathogens. They play a crucial role in preventing bacterial invasion by binding to bacterial components, such as surface proteins or toxins, and marking them for destruction by other immune cells. Deficiencies in antibody production, such as those caused by a weakened B cell function, can impair the body’s ability to neutralize invading bacteria, allowing them to establish infection more easily.
Genetic Variations and Host Susceptibility to Invasion
Host genetic variations can also influence susceptibility to bacterial invasion. Polymorphisms, or variations in specific genes, can affect the expression or function of immune proteins, including those involved in phagocytosis, complement activation, and antibody production. Genetic variations that result in impaired immune function can increase the risk of bacterial infections and make individuals more susceptible to severe disease outcomes.
Understanding the impact of host immune deficiencies on the efficiency of bacterial invasion is crucial for developing effective strategies to prevent and treat infections. By targeting immune deficiencies and enhancing immune function, we can reduce the burden of bacterial diseases and improve patient outcomes.
Replication: The Key to Pathogen Survival
In the relentless battle between pathogens and their host, replication plays a pivotal role in the pathogen’s ability to establish and maintain infection. Bacteria, the microscopic invaders, possess a unique and intricate process of cell division that ensures their survival and the perpetuation of their malicious intents.
At the heart of bacterial replication lies the division of its single, circular chromosome. This critical genetic material, carrying the blueprint for the pathogen’s existence, is meticulously copied and partitioned into two identical daughter cells. Like a delicate dance, the chromosome undergoes a series of intricate movements, guided by a complex machinery of proteins.
The timing of replication is also of utmost importance. Bacteria have evolved to exploit specific moments in the host’s cellular cycle, maximizing their chances of successful multiplication. Their ability to align their replication with the host’s cell division ensures that the newly formed daughter cells can inherit the nutrients they need to thrive.
However, the host is not a passive bystander in this relentless battle. Its immune defenses constantly seek to thwart the pathogen’s replication. Antibiotics, potent weapons in the fight against infection, target specific steps in the bacterial replication process, disrupting their ability to divide and propagate.
The efficiency of bacterial replication has profound implications for pathogen survival. Rapidly replicating bacteria can quickly overwhelm the host’s immune defenses, leading to severe disease. Conversely, impaired replication can significantly reduce the pathogen’s virulence, leading to milder infections or even clearance by the host’s immune system.
Understanding the nuances of bacterial replication is crucial in the fight against infectious diseases. By unraveling the mechanisms that govern this process, scientists can develop novel therapeutic strategies that effectively target and inhibit bacterial replication, ultimately reducing their ability to cause harm and improving patient outcomes.
Influence of Host Factors on Bacterial Replication
The ability of bacteria to replicate within a host is a crucial determinant of disease severity and progression. Host factors play a significant role in modulating bacterial replication, influencing the outcome of infections.
Antibiotics:
- Antibiotics, essential tools in combating bacterial infections, work by disrupting bacterial replication.
- They can inhibit protein synthesis, block cell wall formation, or damage DNA, rendering bacteria incapable of dividing.
- Host factors, such as antibiotic susceptibility and resistance, influence the effectiveness of antibiotics.
Host Defense Mechanisms:
- The immune system is a critical host defense mechanism against bacterial infections.
- Immune cells produce antibodies that neutralize bacteria and activate other immune responses to destroy them.
- Certain genetic factors and immune deficiencies can impair the host’s ability to control bacterial replication.
Host Environment:
- The physiological environment of the host also influences bacterial replication.
- Temperature, pH, and nutrient availability can affect bacterial growth and replication rates.
- Some bacteria have evolved adaptations to thrive in specific host environments, enhancing their ability to replicate and cause disease.
Understanding the influence of host factors on bacterial replication is crucial for developing effective strategies to prevent and treat infections. By targeting these factors, such as improving host immunity or optimizing antibiotic use, we can mitigate the impact of bacterial pathogens and promote overall health.
Host Susceptibility to Pathogens: Understanding the Host’s Role in Disease
In the intricate world of infectious diseases, the battle between pathogen and host is a delicate dance, where the outcome can hinge on the subtlest of factors. Host susceptibility plays a pivotal role in determining whether a pathogen can establish an infection, cause disease, and ultimately threaten our health.
Pathogenicity refers to a pathogen’s ability to cause disease, while virulence measures the severity of that disease. These intertwined concepts are the driving forces behind the wide spectrum of infectious diseases we encounter. Some pathogens, like the common cold virus, are relatively benign, causing mild symptoms that may not require medical intervention. Others, like the Ebola virus, possess immense virulence, leading to devastating outbreaks with high mortality rates.
Pathogenicity and virulence are influenced by an array of factors, including the presence of toxins, the ability to resist antibiotics, and the host’s immune response. Toxins are molecules produced by pathogens that can damage or kill host cells, making infection more severe. Antibiotic resistance, on the other hand, allows pathogens to evade the effects of antimicrobial drugs, rendering them harder to treat. The host’s immune system serves as a formidable defense mechanism, but its effectiveness can vary depending on genetic factors, nutritional status, and immune deficiencies.
Understanding the mechanisms of pathogenicity and virulence is crucial for disease prevention and treatment. By identifying the key virulence factors of a particular pathogen, scientists can develop targeted therapies that neutralize their toxic effects or enhance the host’s immune response. Moreover, understanding the genetic basis of pathogen-host interactions can help predict which individuals are at higher risk of severe disease and guide tailored interventions.
Bacterial Toxins and Antibiotic Resistance: The Deadly Duo of Virulence
In the intricate dance between pathogens and their hosts, bacterial toxins and antibiotic resistance play pivotal roles in shaping the severity of disease. Toxins, potent molecules produced by bacteria, are veritable weapons that disrupt host cells, causing inflammation, tissue damage, and, in severe cases, even death.
The insidious effects of toxins are evident in the infamous Shiga toxin, produced by the bacterium Escherichia coli. This toxin hijacks cells, destroying the very machinery responsible for protein synthesis, leading to cell death and the dreaded symptoms of Shiga toxin-producing E. coli infections.
Antibiotic resistance, another formidable barrier to effective treatment, arises when bacteria develop the ability to withstand the onslaught of antibiotics. This resistance can result from mutations that alter the target sites of antibiotics, blocking their effectiveness. The rise of antibiotic-resistant superbugs, such as methicillin-resistant Staphylococcus aureus (MRSA), has become a major global health concern.
The interplay between toxins and antibiotic resistance compounds the challenge of combating infections. Bacteria that produce toxins are more likely to cause severe disease, and those that are resistant to antibiotics can prolong infections and complicate treatment. This deadly duo underscores the urgent need for ongoing research and development of new strategies to combat bacterial infections.
How the Immune System Shapes the Severity of Disease
When pathogens, those microscopic invaders, breach our defenses, our immune system steps up to the plate like a seasoned warrior. Its job is not just to eliminate these invading foes but also to determine the severity of the battle that ensues.
The immune system is a complex symphony of cells, proteins, and chemicals that work together to neutralize pathogens. But it’s not a one-size-fits-all response. The host’s immune response, unique to each individual, plays a crucial role in determining how virulent a pathogen is—how severe the symptoms it causes can be.
Certain host factors, such as genetic variations, can predispose individuals to severe infections. For instance, some people lack certain antibodies that effectively combat specific pathogens. When such pathogens strike, the immune system struggles to contain them, leading to more severe symptoms.
Chronic diseases, like diabetes or HIV, can also weaken the immune system, making individuals more vulnerable to opportunistic infections, pathogens that normally don’t cause illness. In these cases, the immune system’s ability to fight off invaders is compromised, allowing pathogens to gain a foothold and wreak havoc.
However, the immune system is not always the enemy. Sometimes, its response can be too aggressive, causing autoimmune diseases. In these conditions, the immune system mistakenly attacks the body’s own tissues, leading to inflammation, tissue damage, and potentially fatal consequences.
The delicate balance of the immune system is essential for maintaining our health. When it functions optimally, it can swiftly neutralize pathogens and minimize symptoms. But when host factors interfere with its effectiveness, the severity of an infection can escalate, highlighting the profound influence of the immune system in shaping the course of disease.
Host Specificity in Pathogens: A Tale of Evolution and Adaptation
In the intricate tapestry of life, pathogens and hosts engage in an evolutionary dance, each seeking to outwit the other. One fascinating aspect of this interplay is host specificity, the ability of certain pathogens to exclusively infect and thrive within specific species or groups of species.
Like a tailored key fitting into a lock, pathogens have evolved unique mechanisms that allow them to recognize and gain access to their preferred hosts. These mechanisms can be as intricate as a molecular handshake, where the pathogen’s surface molecules bind to specific receptors on the host’s cells.
But what drives pathogens to evolve such host specificity? The answer lies in the selective pressures encountered in their environments. Pathogens that specialize in infecting a limited range of hosts may enjoy a competitive advantage by avoiding competition from other pathogens that target a broader range of species.
For example, the human immunodeficiency virus (HIV) has evolved to target only human cells, ensuring its survival and perpetuation within this specific host species. In contrast, the influenza virus has a broad host specificity, infecting not only humans but also birds and other animals, which allows it to circulate widely and cause global pandemics.
Understanding the mechanisms behind host specificity is crucial for developing effective strategies to prevent and treat infectious diseases. By deciphering the molecular interactions that govern this specificity, scientists can design targeted interventions that block pathogen entry or disrupt their ability to thrive within specific hosts.
In conclusion, host specificity in pathogens is a testament to the evolutionary arms race between microorganisms and their hosts. By unraveling the intricate mechanisms that underlie this specificity, we can gain valuable insights into the prevention and treatment of infectious diseases, safeguarding human and animal health from the ever-evolving threats of microbial pathogens.
Host Tropism: The Evolutionary Tale of Pathogen Specificity
In the intricate dance between pathogens and their hosts, host tropism plays a pivotal role. It’s the pathogen’s ability to preferentially colonize and cause disease in certain hosts, leaving others relatively unscathed. This selective targeting has profound implications in the realm of infectious diseases.
Host tropism is an evolutionary adaptation that arises from coevolution between pathogens and their hosts. Over eons, pathogens have evolved specific mechanisms to recognize and interact with receptors present on host cells. This molecular finesse allows them to establish a foothold and exploit the host’s resources for their survival and replication.
However, the story doesn’t end there. Host species, too, have evolved counter-measures to protect themselves from these invaders. They develop immune responses that recognize and neutralize pathogens, creating barriers to infection. Consequently, some pathogens may have evolved to overcome these defenses, leading to a continuous arms race between pathogens and their hosts.
The consequences of host tropism are far-reaching. Zoonoses, diseases that can be transmitted from animals to humans, highlight the impact of host specificity. When pathogens jump species, they can encounter hosts with different immune systems and cell receptors. This can lead to unpredictable outcomes, as the pathogen may be more or less virulent in its new host.
Moreover, host tropism influences the severity and duration of infections. Pathogens that are highly adapted to their host tend to cause more severe disease, while those with broader host ranges may result in milder infections. This can have implications for both public health and clinical management.
By understanding the mechanisms and consequences of host tropism, researchers can gain valuable insights into the evolution and epidemiology of infectious diseases. This knowledge can guide the development of targeted therapies that exploit the specific dependencies of pathogens on their host cells.
Host Genetic Variations and Immune Responses: Shaping Host Tropism in Pathogens
When pathogens encounter a host, host factors play a pivotal role in determining their susceptibility to infection. Among these factors, genetic variations and immune responses stand out as key players in shaping host tropism, the preferential targeting of specific hosts by pathogens.
Genetic variations within a host population can profoundly impact pathogen tropism. Certain genetic traits, such as receptor mutations or immune deficiencies, may render hosts more susceptible to particular pathogens. For instance, individuals with a mutation in the CCR5 receptor are less susceptible to HIV infection. Conversely, genetic variations that enhance immune function, such as the presence of HLA-B27 allele, can confer resistance to certain infections.
Immune responses also exert a significant influence on host tropism. A robust innate immune system can effectively recognize and eliminate pathogens before they establish infection. Adaptive immune responses, such as antibody production and cell-mediated immunity, further contribute to host protection. However, pathogens have evolved various mechanisms to evade or suppress immune responses, allowing them to successfully infect and colonize specific hosts.
For example, Neisseria meningitidis can evade the bactericidal effects of the complement system by modifying its surface antigens. Mycobacterium tuberculosis can survive within macrophages, eluding the immune system’s surveillance. These selective advantages, coupled with genetic variations and immune responses, shape the host tropism of pathogens.
Understanding the influence of host genetic variations and immune responses on host tropism is crucial for developing effective disease prevention and treatment strategies. Targeted interventions that bolster immune responses or correct genetic defects could potentially enhance host resistance to specific pathogens. Advances in genomics and immunology are providing valuable insights into these intricate interactions, paving the way for personalized medicine approaches tailored to individual host susceptibilities.
Zoonoses: The Hidden Danger Lurking in Our Animal Companions
Paragraph 1:
Zoonoses, aptly named “diseases of animals that can be transmitted to humans,” often lurk in our furry and feathered friends. The transmission of these pathogens can occur in a variety of ways, depending on the pathogen and the animals involved. Some zoonoses, like rabies, may be transmitted through a bite from an infected animal. Others, such as the infamous bubonic plague, can be carried by fleas or rodents.
Paragraph 2:
The reservoirs for zoonotic pathogens can vary widely. Bats harbor a surprising number of viruses that can be transmitted to humans, including rabies and the more recent COVID-19. Birds, too, can carry diseases like salmonella and avian influenza. Even our beloved house pets, like cats and dogs, can transmit zoonotic diseases such as ringworm, toxoplasmosis, and certain types of bacteria.
Paragraph 3:
Host factors play a crucial role in determining susceptibility to zoonotic diseases. Our immune responses are the first line of defense against invading pathogens. Robust immune systems can help us fight off infections, while compromised immune systems increase our vulnerability. Exposure to animals also influences susceptibility. People who work with animals in professions like veterinary medicine or farming are at higher risk of contracting zoonotic diseases.
Paragraph 4:
Understanding the factors that contribute to zoonotic disease susceptibility is essential for preventing and treating these infections. By practicing good hygiene, avoiding contact with animals that may be carrying diseases, and seeking medical attention promptly if symptoms arise, we can reduce our risk of infection. Additionally, vaccinations for both animals and humans can be an effective way to prevent the spread of certain zoonotic diseases.
Reservoirs and Maintenance of Zoonotic Pathogens
Embrace the Wild: The Silent Symphony of Hosts
In the intricate dance of life, pathogens find their stage in the bustling metropolis of the animal kingdom. These silent orchestrators can reside within a wide spectrum of hosts, ranging from the cuddly companions we adore to the wild creatures that roam the untamed landscapes. These hosts serve as reservoirs, harboring the pathogens without succumbing to their sinister melodies.
A Trove of Microbial Havens
Zoonotic pathogens, those capable of crossing the species barrier to infect humans, find refuge in a diverse array of reservoirs. This enigmatic cast includes domesticated animals, wildlife, and even insects and ticks. Farm animals, such as cattle and pigs, can unknowingly carry pathogens that can leapfrog into our own bodies. Wildlife, such as rodents and bats, can harbor pathogens that may emerge as global pandemics.
The Silent Guardians: Immune Sentinels at Play
The immune systems of reservoir hosts play a pivotal role in maintaining zoonotic pathogens. They have evolved to coexist with these pathogens, often without developing severe symptoms. This delicate balance, however, can be upended by human encroachment or environmental changes, leading to the spillover of pathogens into human populations.
Unraveling the Secrets of Pathogen Persistence
Within their reservoirs, zoonotic pathogens employ a repertoire of strategies to ensure their survival. Some form reservoirs within specific organs or tissues, while others reside in the gastrointestinal tract, constantly shedding into the environment. The ability of pathogens to adapt to their host species and evade immune responses is crucial for their long-term persistence.
A Journey of Discovery: The Promise of Research
Understanding the reservoirs and maintenance of zoonotic pathogens is a scientific quest of paramount importance. Through research, we can unravel the hidden connections between animals, humans, and pathogens. This knowledge will empower us to develop targeted strategies to prevent and control zoonotic diseases, protecting both human and animal health for generations to come.
Host Factors and Zoonotic Disease Susceptibility: A Vital Connection
Zoonotic diseases, those transmitted between animals and humans, pose a significant public health concern. Understanding the factors that influence host susceptibility to these pathogens is crucial for effective disease prevention and management.
Immune Responses and Zoonotic Disease Severity
The immune system plays a pivotal role in controlling zoonotic infections. A robust immune response can quickly identify and eliminate invading pathogens, preventing disease development. However, in individuals with weakened immune systems, such as those with HIV/AIDS or undergoing immunosuppressive therapies, susceptibility to zoonotic pathogens increases. Their compromised immunity hampers the body’s ability to mount a timely and effective defense, allowing pathogens to establish infection and cause disease.
Animal Exposure and Contact with Reservoirs
Exposure to animals infected with zoonotic pathogens is a critical risk factor for human infection. Contact with pets, livestock, wildlife, or contaminated animal products can transmit pathogens to humans through direct contact, bites, or inhalation of infectious aerosols. Individuals who work in animal-related occupations or live in areas with high animal populations are at an increased risk of exposure and subsequent infection.
Examples of Host Factors Influencing Zoonotic Disease Susceptibility:
- Rabies: Susceptibility to rabies is influenced by immune status. Individuals with weakened immune systems or those who fail to receive timely post-exposure prophylaxis are at a higher risk of developing severe disease.
- Hantavirus: Exposure to infected rodents is a major risk factor for hantavirus infection. Individuals who handle rodents or live in areas with high rodent populations are more likely to acquire the virus and develop potentially fatal respiratory or renal syndromes.
- Ebola: Weakened immune systems, such as those of the elderly or those with underlying medical conditions, increase susceptibility to Ebola virus infection. Contact with infected animals or contaminated fluids can transmit the virus, leading to severe hemorrhagic fever and high mortality rates.
Understanding the role of host factors, particularly immune responses and animal exposure, in zoonotic disease susceptibility is essential for protecting public health. By identifying and addressing these risk factors, we can develop targeted prevention strategies and interventions to reduce the incidence and severity of zoonotic infections. Continued research in this area is vital for developing effective measures against these emerging and evolving threats.
The Role of Vectors in Arthropod-Borne Diseases
In the intricate tapestry of life, where human and animal realms intertwine, arthropod-borne diseases emerge as a formidable threat, silently lurking in the shadows of our daily existence. These diseases, transmitted by seemingly innocuous insects and arachnids, have the power to inflict a wide array of illnesses, from the debilitating dengue fever to the potentially fatal malaria.
Vectors, the unwitting carriers of these pathogens, serve as bridges between infected animals and susceptible humans. Mosquitoes, ticks, and fleas are just a few examples of the diverse group of arthropods that can play this perilous role. The transmission process begins when the vector takes a blood meal from an infected animal, ingesting the pathogen along with it.
Within the vector’s body, the pathogen replicates, multiplying its numbers before being transmitted to a new host. This intricate dance between pathogen and vector is influenced by a multitude of factors, including the species of vector, the pathogen’s virulence, and the vector’s immune response.
The complex interplay between vectors and pathogens shapes the epidemiology of arthropod-borne diseases. Mosquitoes, for instance, thrive in warm, humid climates, explaining why dengue fever and malaria are prevalent in tropical regions. Climate change, deforestation, and urbanization are all factors that can alter vector distribution and abundance, potentially leading to increased disease transmission.
Understanding the role of vectors in arthropod-borne diseases is paramount in developing effective control measures. Vector surveillance, habitat modification, and personal protective measures, such as mosquito nets and insect repellents, are all essential strategies in reducing disease risk.
In conclusion, vectors play a pivotal role in the transmission of arthropod-borne diseases, acting as conduits between infected animals and susceptible humans. By unraveling the intricacies of vector-pathogen interactions, we can gain a deeper understanding of disease epidemiology and develop tailored interventions to protect ourselves from these insidious threats.
Factors Influencing Vector-Host Interactions: A Tale of Survival
In the intricate dance between pathogens, vectors, and hosts, understanding vector-host interactions is paramount. These tiny creatures, often overlooked but wielding immense power, serve as crucial intermediaries, carrying pathogens from one host to another. Yet, the success of this partnership hinges on a complex interplay of factors that shape the dynamics of infection.
One such factor is vector competence. This attribute refers to the ability of a vector to acquire, maintain, and transmit pathogens efficiently. Variations in vector competence arise from species-specific adaptations, such as anatomical features that facilitate pathogen uptake or physiological mechanisms that support their survival within the vector.
Host susceptibility also plays a pivotal role. Vectors exhibit preferences for particular hosts, based on factors like skin texture, blood type, and immune responses. Some hosts, known as reservoir hosts, harbor pathogens persistently, serving as sources of infection for vectors.
Environmental conditions exert a significant influence as well. Temperature, humidity, and vegetation can affect vector abundance, activity patterns, and longevity. These factors impact both vector survival and their ability to transmit pathogens.
Vector control measures aim to reduce vector-host interactions. Insecticide spraying, habitat modification, and personal protective measures can disrupt transmission dynamics. However, the success of these strategies depends on understanding the specific vector-host interactions involved in disease spread.
Vector-host interactions are a complex interplay of biological, ecological, and environmental factors that determine the success of pathogen transmission. Understanding these interactions is crucial for developing effective vector control strategies and mitigating the spread of vector-borne diseases.
How Host Factors Influence Disease Transmission by Vectors
Navigating through a pathogen’s journey from one host to another is a complex narrative, where host factors play a pivotal role in determining the outcome. Vectors, such as mosquitoes or ticks, act as intermediaries, shuttling the pathogen between different hosts. Understanding how host factors modulate disease transmission by vectors is crucial for effective disease prevention and control.
Immune Responses
The human immune system stands as a formidable defense against invading pathogens. However, the effectiveness of this defense varies among individuals. Some immune systems are more adept at recognizing and eliminating pathogens, while others may be compromised by diseases, malnutrition, or genetic factors. This variation in immune competence influences the ability of the pathogen to survive and establish an infection within the host.
Vector Avoidance Behaviors
Human behavior can significantly impact disease transmission by vectors. Vector avoidance behaviors, such as wearing protective clothing, using insect repellents, and avoiding areas with high vector activity, can drastically reduce the risk of exposure to infected vectors. Education and awareness about these behaviors are essential in empowering individuals to protect themselves and their communities.
Social and Environmental Factors
Socioeconomic conditions, such as poverty and overcrowding, can also influence disease transmission by vectors. In areas where people live in close proximity to vector habitats, the risk of exposure increases. Access to healthcare, sanitation, and vector control measures are critical in reducing the impact of vector-borne diseases in these vulnerable communities.
Host-Vector Interactions
The interaction between the host and the vector is a delicate dance. Host genetic variations can affect an individual’s susceptibility to infection and the severity of symptoms. For example, certain genetic traits may make individuals more likely to transmit the pathogen to vectors, or to develop severe disease if infected. Understanding these variations can aid in identifying high-risk populations and developing targeted interventions.
Vector Competence
The ability of a vector to transmit a pathogen depends on its vector competence. This competence varies among vector species and can be influenced by factors such as the vector’s feeding habits, lifespan, and ability to replicate the pathogen. Understanding vector competence is crucial for predicting disease transmission patterns and developing effective vector control strategies.
By unraveling the complex interplay between host factors and vector-borne disease transmission, we can strengthen our defenses against these pathogens. Educating communities about vector avoidance behaviors, improving healthcare and sanitation, and continuing research on host-vector interactions are essential steps towards reducing the burden of vector-borne diseases worldwide.
Factors of Host Susceptibility Related to Pathogens: A Comprehensive Analysis
In the realm of disease and infection, host susceptibility plays a pivotal role in determining the fate of interactions between pathogens and organisms. Host factors can dramatically influence the ability of pathogens to adhere, colonize, invade, replicate, and cause disease. This complex interplay between pathogen strategies and host defenses forms the foundation of understanding disease susceptibility.
Adhesion and Colonization
The initial step in infection is adherence, where pathogens establish contact with the host’s tissues. Host receptors serve as docking points for bacterial molecules, facilitating colonization. Mucosal barriers, such as the gut lining, play a crucial role in preventing bacterial invasion. However, immune responses and other host factors can weaken these defenses, increasing susceptibility to colonization.
Invasion
Once colonized, pathogens strive to breach the host’s protective barriers and invade host cells. Invasion mechanisms vary widely, from direct penetration to exploiting cellular pathways. Immune responses, such as phagocytosis, act as barriers to prevent invasion. Host immune deficiencies can compromise these defenses, allowing pathogens to establish intracellular infections.
Replication
Bacterial replication within the host’s cells is essential for pathogen survival and disease progression. Host factors, such as antibiotics and immune responses, can inhibit bacterial replication. Factors like iron availability may influence pathogen growth and virulence, shaping the severity of infection.
Pathogenicity and Virulence
Pathogenicity, the disease-causing ability of a pathogen, and virulence, the severity of the disease it causes, are influenced by various host factors. Bacterial toxins can harm host cells, while antibiotic resistance mechanisms hinder the effectiveness of treatments. The host’s immune system plays a crucial role in modulating pathogenicity and virulence, determining the outcome of infection.
Host Tropism
The ability of pathogens to infect特定 host species is known as host tropism. This specificity arises from the interplay between bacterial molecules and host receptors. Genetic variations and immune responses in the host population can influence host tropism, affecting the distribution of pathogens within and between species.
Zoonoses
Zoonoses are diseases that can be transmitted between animals and humans. Host susceptibility to zoonotic pathogens depends on immune responses, animal exposure, and other host factors. Understanding the factors that influence zoonoses is crucial for preventing their spread and safeguarding public health.
Vectors
Arthropod-borne diseases rely on vector organisms, such as mosquitoes, to transmit pathogens. Vector-host interactions are influenced by immune responses and vector avoidance behaviors. Host factors, such as vector preference and immune protection, can significantly impact disease transmission dynamics.
Factors of host susceptibility related to pathogens are a vast and complex subject. By understanding these factors, researchers and healthcare professionals can better prevent and treat infectious diseases. Future research should focus on unraveling the intricacies of host-pathogen interactions to develop novel interventions and improve patient outcomes.
Emphasize the importance of understanding these factors for disease prevention and treatment
Host Susceptibility: Unveiling the Hidden Factors that Influence Disease Outcomes
In the intricate world of microbiology, the interaction between pathogens and their hosts is a constant battle for survival. While pathogens seek to invade and exploit their hosts, hosts have evolved an array of defense mechanisms to protect themselves. Understanding the factors that influence host susceptibility is crucial for developing effective strategies to prevent and treat infectious diseases.
The Puzzle of Adhesion and Invasion
When a pathogen first encounters a host, it must find a way to attach itself to the host’s cells. This process, known as adhesion, is facilitated by specific receptors on the host’s surface. Once attached, the pathogen can begin to invade the host’s cells, often using specialized enzymes or proteins to penetrate the cell membrane.
Host Factors Shaping the Battleground
The outcome of the pathogen-host interaction is heavily influenced by host factors such as immune responses, mucosal barriers, and genetic variations. A robust immune system can recognize and eliminate pathogens, while a weakened immune system can make the host more susceptible to infection. Additionally, certain variations in host genes can increase or decrease the risk of infection.
Pathogenicity and Virulence: The Keys to Disease Severity
Pathogenicity refers to the ability of a pathogen to cause disease, while virulence describes the severity of the disease. Understanding the factors that contribute to pathogenicity and virulence, such as the production of toxins or antibiotic resistance, is critical for developing effective treatments.
Host Tropism: A Selective Approach
Some pathogens exhibit host tropism, meaning they have a preference for infecting certain hosts or specific cells within a host. This preference is determined by the interplay between the pathogen’s receptors and the host’s unique characteristics. Host genetic variations and immune responses can influence the susceptibility of different individuals to specific pathogens.
Zoonoses: A Bridge Between Animal and Human Health
Zoonoses are diseases that can be transmitted from animals to humans. Understanding the reservoirs of zoonotic pathogens and the factors that influence their transmission, such as animal exposure and immune responses, is crucial for preventing and controlling these diseases.
Vectors: Silent Carriers of Pathogens
Certain pathogens rely on vectors, such as mosquitoes or ticks, to transmit them between hosts. Vector-host interactions are influenced by factors such as the immune responses and avoidance behaviors of the host. By understanding these interactions, we can develop strategies to disrupt disease transmission.
Harnessing Knowledge for Disease Prevention and Treatment
Understanding the factors of host susceptibility related to pathogens provides valuable insights into the development of effective disease prevention and treatment strategies. By manipulating host factors, such as boosting immune responses or modifying genetic susceptibility, we can reduce the risk of infection and improve patient outcomes.
Future Frontiers in Host Susceptibility Research
Continued research in host susceptibility will lead to a deeper understanding of the mechanisms by which pathogens interact with hosts. This knowledge will fuel advancements in personalized medicine, tailored treatments, and innovative strategies to combat emerging infectious diseases. By unraveling the mysteries of host susceptibility, we empower ourselves to protect our health and the health of generations to come.
Factors of Host Susceptibility Related to Pathogens: A Comprehensive Outline
Understanding host factors that contribute to pathogen susceptibility is crucial for disease prevention and cure. These factors influence the course of infection, from adhesion and colonization to invasion, replication, and pathogenicity.
Adhesion and Colonization:
Pathogens adhere to host cells using receptors that mediate attachment. The formation of biofilms further strengthens colonization, shielding pathogens from host immune responses.
Invasion:
Pathogens breach host cell barriers through various mechanisms. Immunity deficiencies and disrupted cell signaling can facilitate invasion, compromising host defense.
Replication:
Pathogen division is essential for survival. Host defense mechanisms and antibiotics can limit replication, hindering pathogen spread.
Pathogenicity and Virulence:
Pathogens cause disease through toxins and antibiotic resistance. Host immune systems play a vital role in modulating virulence, influencing disease severity.
Host Tropism:
Pathogens exhibit a preference for specific hosts. Genetic variations and immune responses influence host tropism.
Zoonoses:
Pathogens can cross species barriers, causing zoonoses. Reservoirs and animal exposure contribute to zoonotic disease susceptibility.
Vectors:
Arthropods transmit pathogens between hosts. Host immune responses and vector avoidance behaviors impact disease transmission.
Future Research Directions:
- Host-Pathogen Coexistence: Studying how hosts and pathogens coexist and evolve.
- Precision Medicine: Developing individualized therapies based on host susceptibility profiles.
- Antimicrobial Resistance: Addressing the growing threat of antibiotic resistance.
- Vector Control: Exploring innovative strategies to control vector-borne diseases.
- Surveillance and Epidemiology: Monitoring pathogen emergence and host susceptibility patterns.
By unraveling the complex interplay between host susceptibility and pathogens, we can revolutionize disease prevention and treatment, safeguarding human and animal health from infectious threats.