Hemostasis: Understanding The Body’s Bleeding Control Mechanisms For Seo
Upon blood vessel injury, the body’s immediate response aims to prevent excessive bleeding through a series of processes. Vasoconstriction, the narrowing of blood vessels, restricts blood flow to the injured area. Platelets, triggered by thrombin and ADP, adhere to the damaged vessel and aggregate to form a platelet plug. This temporary barrier prevents further blood loss. Simultaneously, the coagulation cascade, a complex series of reactions, converts fibrinogen to fibrin, which reinforces the platelet plug, creating a stable fibrin clot and sealing the injury.
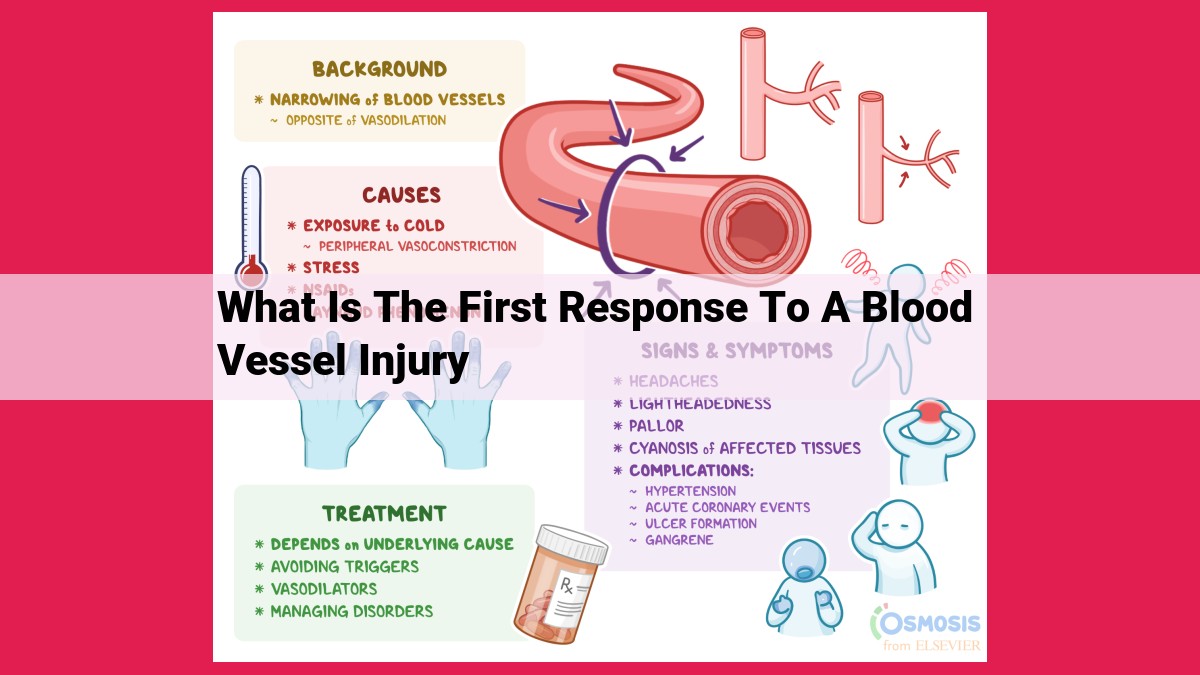
First Response to Blood Vessel Injury: Nature’s Defense Against Bleeding
When the delicate walls of a blood vessel are breached, our bodies swiftly spring into action to prevent excessive bleeding and initiate healing. This intricate process, known as hemostasis, involves a series of precisely coordinated responses that work together to seal the wound and restore the integrity of the circulatory system.
The first line of defense against blood loss is vasoconstriction, the tightening of blood vessels at the site of injury. This constriction reduces blood flow to the damaged area, effectively stemming the tide of blood pouring from the wound. Simultaneously, platelets, small, disk-shaped cells present in the blood, rush to the scene. They become activated by the presence of damaged blood vessels and sticky proteins called von Willebrand factor (VWF). These activated platelets then clump together, forming a temporary plug that further obstructs blood flow and provides a platform for the initiation of more permanent repairs.
This initial response buys the body time to activate the coagulation cascade, a complex series of enzymatic reactions that result in the formation of a fibrin clot. Fibrin is a strong, insoluble protein that weaves a mesh-like network around the platelet plug, reinforcing it and preventing further bleeding. This fibrin clot forms a protective barrier over the wound, ensuring that it remains sealed until the damaged blood vessel can be repaired and the flow of blood can resume normally.
Concept 1: Vasoconstriction – The Body’s Quick-Acting Blood Flow Regulator
When blood vessels are injured, time is of the essence to prevent excessive bleeding. As if by magic, the body initiates a rapid response known as vasoconstriction, a remarkable process that swiftly narrows the damaged blood vessels.
Imagine smooth muscle cells wrapped around these blood vessels like tiny rubber bands. Upon injury, these muscle cells receive a chemical signal, prompting them to contract. As they clench tighter, the blood vessel’s diameter decreases, effectively reducing the flow of blood to the damaged area.
This constriction is a crucial step in minimizing blood loss. By constricting the blood vessels, the body slows down the flow of blood and allows other mechanisms, such as platelet activation and clotting, to kick into gear.
Platelet Activation and Aggregation: The Body’s Defense against Excessive Bleeding
Activation of Platelets: From Bystanders to First Responders
Blood vessel injuries, no matter how seemingly minor, can trigger a cascade of rapid and efficient responses within the body. One of the key players in this response is the activation of platelets, tiny blood cells responsible for plugging damaged vessels and preventing excessive blood loss.
The activation of platelets is a complex process involving multiple factors. The first step is the release of thrombin, an enzyme that plays a crucial role in the coagulation cascade. Thrombin binds to platelet receptors, triggering a change in shape and the release of messenger molecules like ADP from the platelet’s granules.
ADP: A Powerful Platelet Activator
ADP, short for adenosine diphosphate, is a potent platelet-activating agent. It acts as an amplifier, further enhancing the activation of platelets. ADP binds to its specific receptors on platelets, causing them to undergo a series of conformational changes that ultimately culminate in platelet aggregation, the process of sticking together to form a protective plug.
VWF: The Glue that Holds Platelets Together
Von Willebrand factor (VWF) is a large protein that plays a vital role in the adhesion of platelets to damaged blood vessels. VWF binds to both the damaged vessel’s surface and the platelet’s membrane, creating a molecular bridge that helps platelets aggregate and form a stable plug. Without VWF, the platelet plug would be less effective in sealing the damaged vessel.
The Importance of Platelet Activation and Aggregation
The activation and aggregation of platelets are essential processes for controlling bleeding and promoting healing. By working together, these tiny blood cells form a platelet plug that acts as a temporary barrier against blood loss. This plug initiates the formation of a more permanent clot through the activation of the coagulation cascade, discussed in the next section of this blog post series.
Concept 3: Formation of a Platelet Plug
In response to a blood vessel injury, the body’s first line of defense is to vasoconstrict, activate platelets, and form a platelet plug. This plug acts as a temporary seal to prevent excessive bleeding while the more complex coagulation cascade kicks in.
Hemostasis, the process of stopping blood loss, is crucial to maintaining the body’s integrity. Platelets, small, disk-shaped blood cells, play a pivotal role in this process by adhering to the damaged vessel walls and forming a physical barrier against bleeding.
Platelet Activation and Aggregation
Once platelets come into contact with the damaged blood vessel, they become activated and undergo a shape change. They extend pseudopodia, finger-like projections, which allow them to attach to the injured vessel lining. This is facilitated by a protein called von Willebrand factor (VWF), which acts as a bridge between platelets and the damaged tissue.
As platelets adhere to the site of injury, they release chemical signals that attract more platelets to the area. These signals include thrombin and ADP (adenosine diphosphate), which activate nearby platelets, causing them to aggregate and form clumps. The growing platelet aggregate forms the foundation of the platelet plug.
Reinforcement of the Platelet Plug
The platelet plug is not just a passive barrier; it becomes reinforced over time. As more platelets accumulate, they release more thrombin, which converts fibrinogen, a soluble protein in the blood, into insoluble fibrin strands. These fibrin strands form a mesh-like network around the platelet aggregate, further strengthening the plug and stabilizing the clot.
The formation of a platelet plug is a critical step in the body’s response to blood vessel injury. It provides a temporary seal, preventing excessive bleeding and giving the coagulation cascade time to amplify the clotting response and form a more permanent clot.
Concept 4: Activation of the Coagulation Cascade and Formation of a Fibrin Clot
As the body races against time to halt the flow of precious lifeblood, a complex series of reactions known as the coagulation cascade springs into action. This intricate dance of biochemical events involves a multitude of proteins, each playing a specific role in orchestrating the formation of a sturdy fibrin clot.
At the heart of this cascade lies thrombin, a pivotal enzyme that catalyzes the conversion of fibrinogen, a soluble protein, into insoluble fibrin strands. These newly formed fibrin strands intertwine, forming a mesh-like network that reinforces the platelet plug, creating an impenetrable barrier against further bleeding.
The coagulation cascade is activated through two distinct pathways: the intrinsic pathway and the extrinsic pathway. The intrinsic pathway is triggered when factor XII, a protein found in blood plasma, comes into contact with a damaged blood vessel. The extrinsic pathway, on the other hand, is initiated by tissue factor, a protein released from damaged cells lining the blood vessel.
Once either pathway is activated, a cascade of reactions ensues, culminating in the formation of thrombin. This intricate process involves the sequential activation of various clotting factors, each catalyzing the conversion of the next in a domino-like effect.
The final step in this cascade involves thrombin acting on fibrinogen, cleaving it into fibrin monomers. These monomers then spontaneously polymerize, forming a network of fibrin strands that interlace with the platelet plug. This fibrin clot provides additional strength and stability, ensuring that the bleeding vessel remains sealed.