Braden Scale: Identify And Prevent Pressure Sore Risk With Comprehensive Assessment
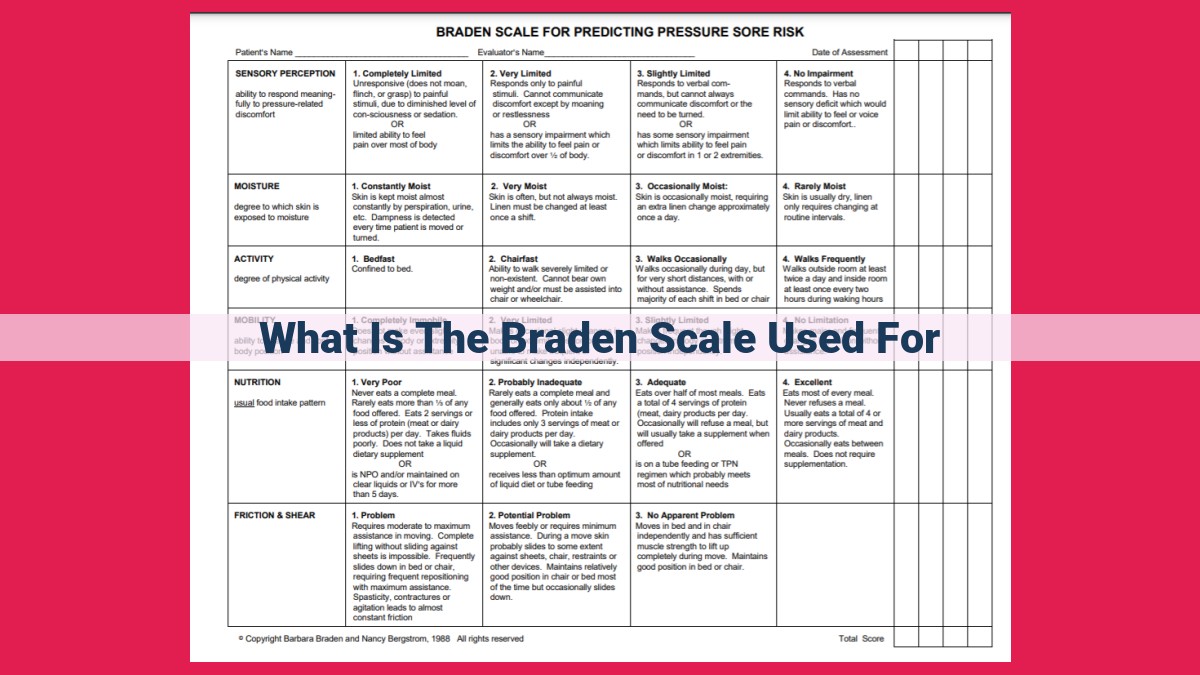
The Braden Scale is a risk assessment tool used to identify patients at risk of developing pressure ulcers. It assesses six factors: sensory perception, moisture, activity, mobility, nutrition, and friction/shear. A score of 18 or less indicates a high risk of developing a pressure ulcer, and interventions should be implemented to prevent its development.
Understanding Pressure Ulcer Risk
In the realm of healthcare, preventing and managing pressure ulcers is a crucial aspect of patient care. Pressure ulcers, also known as bedsores, are localized injuries to the skin and underlying tissues caused by prolonged pressure on the body. Understanding the risk factors associated with pressure ulcers is essential in preventing their development.
Risk Factors:
- Immobility: Individuals who are bedridden or have limited mobility have an increased risk of developing pressure ulcers.
- Shear forces: Sliding or dragging the body against surfaces can create friction and lead to pressure ulcers.
- Medical conditions: Certain health conditions, such as diabetes, malnutrition, and neurological disorders, can impair circulation and increase susceptibility to pressure ulcers.
- Age: The skin becomes thinner and more fragile with age, making elderly individuals more prone to pressure ulcers.
- Weight: Obese patients have a higher risk due to increased pressure on the skin and tissues.
Assessing Risk:
Early identification of high-risk patients is vital for effective prevention. Healthcare professionals use risk assessment tools, such as the Braden Scale or Norton Scale, to evaluate factors like mobility, sensory perception, and nutritional status. These tools help categorize patients into high-risk, medium-risk, or low-risk groups, allowing for targeted interventions.
Identifying Patients at Risk: Uncovering Signs and Symptoms for Prevention
Understanding who is vulnerable to pressure ulcers is crucial for effective prevention. Certain physical and behavioral characteristics can serve as early warning signs.
Physical Indicators:
- Immobility: Extended periods of lying or sitting without frequent repositioning increase pressure on specific body areas.
- Skin Integrity: Thin, fragile skin, or areas with previous damage are more susceptible to pressure ulcers.
- Nutritional Deficiencies: Malnutrition, dehydration, and vitamin deficiencies weaken the skin and underlying tissues.
- Neurological Impairments: Conditions like spinal cord injuries or paralysis can reduce sensation, impairing the ability to detect pressure discomfort.
Behavioral Characteristics:
- Incontinence: Constant moisture from urine or feces can soften the skin, making it more vulnerable to breakdown.
- Smoking: Nicotine constricts blood vessels, reducing oxygenation and nutrients to the skin.
- Poor Hygiene: Unclean skin harbors bacteria and increases the risk of infection.
- Age: Elderly individuals often have thinner skin and reduced mobility, increasing their risk.
Screening Methods:
Early detection is paramount. Visual inspection and physical exams can identify potential pressure ulcer sites and assess risk factors.
Visual Inspection:
- Examine skin for redness, swelling, or open wounds.
- Note areas of increased moisture or maceration.
- Check for bony prominences and potential pressure points.
Physical Examination:
- Assess skin integrity, turgor, and hydration.
- Evaluate mobility and sensation in high-risk areas.
- Determine nutritional status and known medical conditions.
By understanding the physical and behavioral characteristics associated with pressure ulcer risk and employing effective screening methods, healthcare professionals can identify high-risk individuals and initiate timely preventive interventions.
Developing Preventive Interventions: A Holistic Approach to Preserving Skin Health
Preventing pressure ulcers, commonly known as bedsores, requires a comprehensive approach that targets both underlying risk factors and daily care practices. Evidence-based strategies, national guidelines, and patient empowerment play crucial roles in this preventive mission.
Evidence-Based Strategies: A Toolkit for Prevention
Repositioning, support surfaces, and proper nutrition form the core of evidence-based strategies for pressure ulcer prevention. Repositioning involves regularly shifting the patient’s body weight to relieve pressure points, particularly over bony prominences. Support surfaces, such as specialty mattresses and cushions, provide optimal pressure distribution, reducing the risk of skin breakdowns. Adequate nutrition, rich in protein and vitamins, supports skin health and wound healing.
Adhering to Guidelines: A Roadmap for Best Practices
National and international guidelines, such as those from the National Pressure Ulcer Advisory Panel (NPUAP), provide a standardized framework for pressure ulcer prevention. These guidelines encompass risk assessment protocols, recommended repositioning schedules, and nutritional guidelines. By adhering to these standards, healthcare professionals ensure consistent and effective prevention practices.
Patient Education and Self-Care: Empowering Individuals
Educating patients about their role in pressure ulcer prevention is essential. Involving them in care decisions and teaching them self-care techniques, such as skin inspection, repositioning, and pressure relief, empowers them to take ownership of their well-being. Self-care empowers individuals to make informed choices that support skin health and minimize the risk of pressure ulcers.
Monitoring Patient Progress: Detecting and Intervening to Prevent Pressure Ulcers
Continuous Monitoring for Early Intervention
Maintaining vigilance is crucial in the fight against pressure ulcers. Establishing a regular monitoring routine enables you to detect any developing issues before they escalate. Visual inspection remains a cornerstone of this process, allowing you to assess the skin’s condition for telltale signs of redness, swelling, or warmth—all early warning indicators that require prompt attention.
Understanding Early Warning Signs
Beyond these visible cues, it’s essential to be mindful of other indicators that may signal impending pressure ulcer formation. Pain, itching, or numbness in pressure-prone areas should not be ignored. These sensations can manifest long before any skin changes appear, providing a valuable window of opportunity for intervention.
Documenting Observations for Optimal Care
Detailed documentation is vital for tracking patient progress and informing timely treatment decisions. Carefully record the location, size, and appearance of any suspected pressure ulcers, along with any associated symptoms. These observations will serve as an invaluable reference point for monitoring changes over time.
Evaluating the Effectiveness of Pressure Ulcer Prevention Interventions
Understanding the effectiveness of pressure ulcer prevention interventions is crucial to ensure optimal patient outcomes. Key outcome measures are used to objectively assess the impact of these interventions. These include:
- Ulcer incidence rates: The number of new pressure ulcers developed over a specific period, providing an indication of the overall efficacy of prevention strategies.
- Average number of ulcers per patient: This metric measures the prevalence of pressure ulcers within a population and can indicate the severity of the problem.
- Time to ulcer development: The duration from the start of the intervention to the onset of a pressure ulcer, which can provide insights into the responsiveness of patients to preventive measures.
In addition to outcome measures, it is vital to employ appropriate study designs and analysis methods to evaluate pressure ulcer prevention interventions. Randomized controlled trials (RCTs) are considered the gold standard for assessing the effectiveness of interventions. RCTs involve randomly assigning participants to an intervention group or a control group to minimize bias and ensure valid comparisons.
Statistical analysis methods are used to analyze data collected from intervention studies. Common techniques include:
- Univariate analysis: Compares the outcome measures between the intervention and control groups, identifying significant differences.
- Multivariate analysis: Considers multiple factors simultaneously to determine their combined effect on pressure ulcer development.
By carefully evaluating the effectiveness of pressure ulcer prevention interventions using key outcome measures and appropriate study designs and analysis methods, healthcare professionals can identify effective strategies and make informed decisions to improve patient care.