Blood Clotting: Positive Feedback Loop Ensures Rapid Clot Formation In Hemostasis
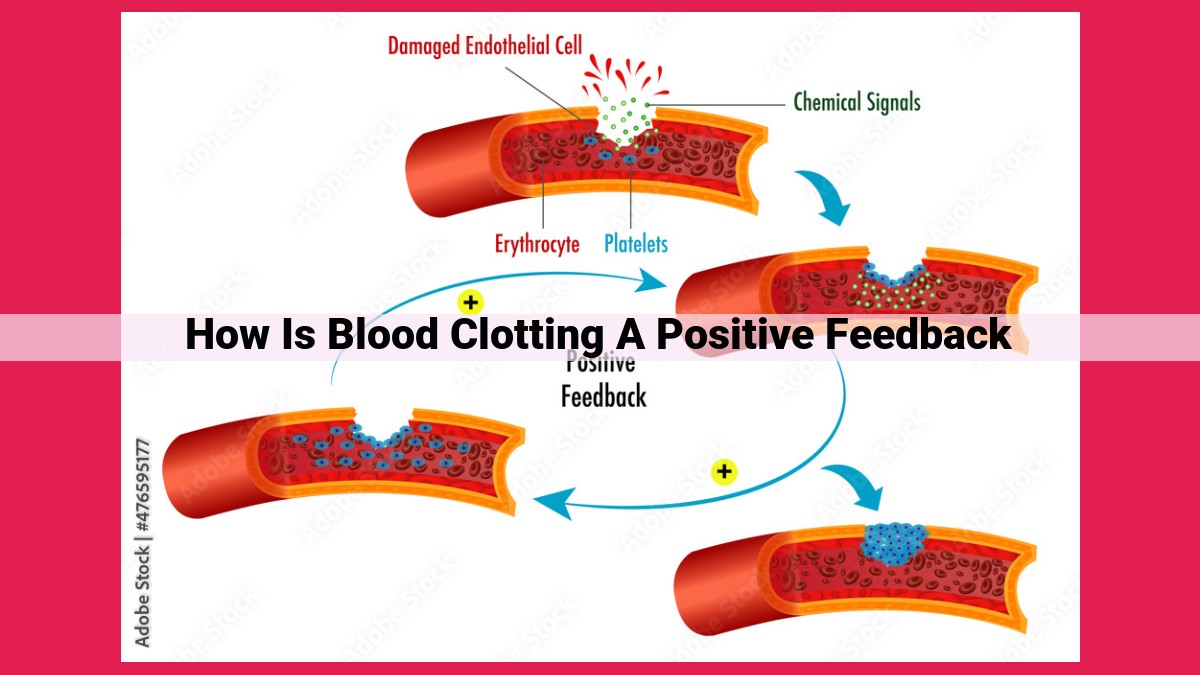
Blood clotting, a vital process to prevent excessive bleeding, relies on a positive feedback loop. When platelets are activated, they release chemical messengers that amplify their response, initiating a cascade of enzymatic reactions. Thrombin, a key enzyme, converts fibrinogen to fibrin, which forms a mesh that traps platelets and red blood cells, creating a stable clot. This positive feedback cycle ensures a rapid and localized response to seal damaged blood vessels, demonstrating the importance of this regulatory mechanism in maintaining hemostasis.
Positive Feedback: The Core of Blood Clotting
- Explain the concept of positive feedback in biological processes and provide an overview of how it applies to blood clotting.
Positive Feedback: The Core of Blood Clotting
Imagine a forest fire, one that doesn’t seem so bad at first. But as it grows, it intensifies, spreading with alarming speed. Positive feedback, a crucial concept in biological processes, is what drives this inferno-like spread, and it also plays a critical role in blood clotting.
Blood clotting is an essential defense mechanism that prevents excessive bleeding after an injury. At its heart lies a cascade of reactions, fueled by positive feedback, that leads to the formation of a stable clot.
Step 1: Platelet Activation – The Initial Trigger
Blood platelets, tiny cell fragments, are the first responders in blood clotting. When a blood vessel is injured, they rush to the site, sticking together to form a temporary plug. As they do, they release chemical messengers, including thromboxane A2, that amplify the response.
Step 2: Thrombin Formation – The Enzyme that Drives the Cascade
The key player in the clotting cascade is thrombin, an enzyme that converts fibrinogen, a soluble protein in the blood, into fibrin. Like a glue, fibrin traps platelets and red blood cells, forming a stable clot.
How does positive feedback come into play? Thrombin not only converts fibrinogen to fibrin but also activates other factors in the cascade, amplifying the production of thrombin. This creates a vicious cycle, leading to the rapid formation of a clot.
Step 3: Fibrin Formation – The Sealant That Completes the Process
As thrombin catalyzes the formation of fibrin strands, they entrap platelets and red blood cells, creating a barrier that prevents further blood loss. This stable clot provides the necessary time for the injured blood vessel to repair itself.
The Importance of Positive Feedback in Blood Clotting
Positive feedback plays a crucial role in blood clotting by promoting a rapid and effective response. Without it, clots would form too slowly or not at all, potentially leading to excessive bleeding and life-threatening complications. Conversely, too much positive feedback, such as in the case of a blood clot in an artery, can result in thrombosis, blocking blood flow and potentially causing serious health issues.
Understanding the intricate balance of positive feedback in blood clotting is essential for scientists and medical professionals alike, as it helps them develop therapies to prevent both excessive bleeding and unwanted clotting.
Step 1: Platelet Activation – The Initial Trigger
In the intricate ballet of blood clotting, platelets emerge as the first responders, initiating a cascade of events that ultimately staunch bleeding. These microscopic disc-shaped cells, ever vigilant in our bloodstream, play a crucial role in preventing excessive blood loss and maintaining vascular integrity. The process of platelet activation, triggered by tissue damage, sets the stage for the intricate symphony of blood clotting.
Upon encountering damaged blood vessels, platelets undergo a remarkable transformation. They change shape from smooth discs to spiky spheres, akin to miniature sea urchins. This conformational change exposes receptors on their surface, allowing them to bind to the exposed collagen in the injured vessel. It’s this binding interaction that initiates platelet activation, the spark that ignites the clotting cascade.
Once activated, platelets release a plethora of chemical messengers, the heralds of the clotting process. These chemical messengers, like tiny messengers in a complex network, amplify the response, attracting more platelets to the site of injury and triggering the release of coagulation factors from the surrounding tissues. The scene is set for the next stage of the clotting saga, the formation of thrombin, the enzyme that drives the cascade.
Step 2: Thrombin Formation – The Enzyme that Drives the Cascade
In the intricate tapestry of blood clotting, thrombin stands as the maestro, orchestrating a cascade of events that transforms liquid blood into a solid clot. This enzyme plays a pivotal role in converting fibrinogen into fibrin, the essential protein that forms the scaffolding of the clot.
Thrombin’s presence sets off a chain reaction, a positive feedback loop, that amplifies the clotting response. As more thrombin is formed, it further activates platelets and promotes the conversion of more fibrinogen to fibrin. This self-reinforcing mechanism ensures a rapid and efficient response to injury, preventing excessive bleeding.
The activation of thrombin is a complex process involving a series of molecular interactions. It begins with the binding of clotting factors to the surface of activated platelets. These factors then undergo a cascade of reactions, culminating in the conversion of prothrombin to thrombin.
Thrombin’s activity is tightly regulated to prevent excessive clotting. Natural anticoagulants in the blood, such as antithrombin III, act as watchdogs, limiting thrombin’s activity and ensuring a delicate balance between clotting and bleeding.
Step 3: Fibrin Formation – The Sealant That Completes the Process
As the blood clotting cascade progresses, the critical enzyme thrombin takes center stage. Its primary mission? To orchestrate the formation of fibrin, the essential sealant that solidifies the nascent clot.
Thrombin, like a master chemist, catalyzes a remarkable transformation. It cleaves fibrinogen, a soluble protein present in blood, into fibrin monomers. These monomers, once released, undergo a dramatic change. They spontaneously polymerize, intertwining and cross-linking to form an intricate web of insoluble fibrin strands.
These strands, like a delicate lacework, entrap platelets and red blood cells within their embrace. As more and more fibrin strands accumulate, a stable meshwork is created, effectively trapping blood components and sealing the damaged blood vessel.
The fibrin meshwork serves as a vital barrier, preventing blood from escaping and ensuring that the healing process can commence. It gradually strengthens over time, further stabilizing the clot and promoting tissue repair.
In essence, fibrin formation represents the culmination of the blood clotting cascade, a testament to the body’s remarkable ability to maintain its integrity and prevent excessive bleeding. Without this final step, the clotting process would remain incomplete, leaving wounds vulnerable and risking further complications.
The Unsung Hero: The Critical Role of Positive Feedback in Blood Clotting
Positive feedback, a phenomenon where the output of a process amplifies the input, plays a starring role in our body’s defense against excessive bleeding: blood clotting. Delving deeper into this intricate process reveals how a simple cut triggers an orchestrated cascade of events, effectively sealing the wound and preventing loss of precious blood.
Platelets, the sentinels of our bloodstream, initiate this intricate dance. When they encounter an injury, they become activated, releasing chemical signals that recruit more platelets to the site. As this army of platelets gathers, they begin to transform themselves into a sticky patchwork, creating a temporary plug that slows down the blood flow.
Thrombin, a molecular maestro, takes center stage next. This enzyme, fueled by the positive feedback loop, converts fibrinogen, a soluble protein, into insoluble fibrin strands. These strands intertwine, forming a net that enmeshes platelets and red blood cells, reinforcing the clot and ensuring its stability.
The positive feedback loop that orchestrates this clotting process is essential for several reasons. First, it accelerates the clotting response, minimizing blood loss. Second, it localizes the clot formation, preventing it from spreading to other areas. Third, it promotes clot stability, ensuring that the sealed wound remains protected until healing is complete.
Without this positive feedback mechanism, blood clotting would be a slow and ineffective process, leaving us vulnerable to uncontrolled bleeding. The body’s ability to harness this feedback loop highlights the remarkable adaptability and resilience of our biological systems, showcasing how our bodies work in harmony to protect us from harm.